Rickettsial diseases are vector-borne, bacterial infections that cause acute febrile illness throughout the world. Because symptoms of rickettsial diseases are often non-specific in nature and overlap with other febrile diseases with similar epidemiology, their diagnosis is challenging. The diagnostic difficulties likely contribute to the historical underreporting of cases of these diseases.
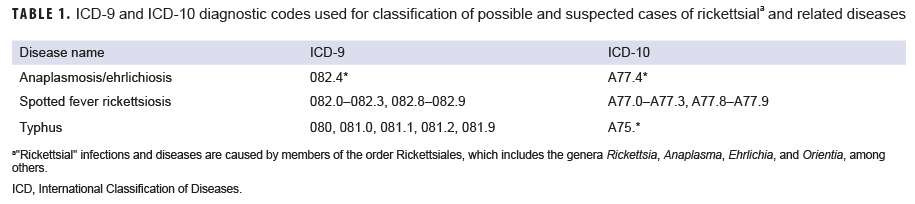
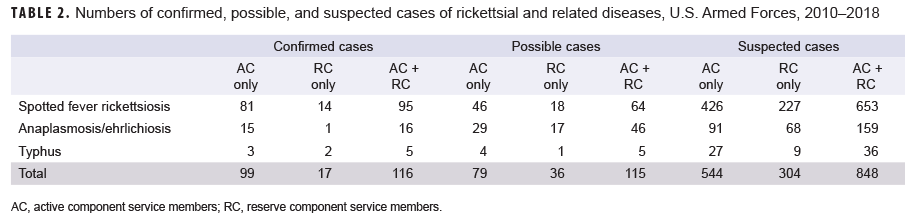
In 2018, the MSMR published a report on the surveillance of vector-borne disease in active and reserve component service members that included estimates of incident cases of rickettsial and related diseases during the surveillance period from 2010 through 2016.1 The analysis for this snapshot used similar methodology but restricted the analysis to rickettsial diseases and extended the surveillance period through 2018. A "confirmed" case was defined as an individual identified through a reportable medical event (RME) report of a rickettsial or related disease that was described as "confirmed" by having met specific laboratory and/or epidemiologic criteria.2 A "possible" case was defined by a record of hospitalization with a diagnosis for a rickettsial disease (Table 1) in any diagnostic position. A "suspected" case was defined by either an RME of a rickettsial disease without laboratory or epidemiologic confirmation or a record of an outpatient medical encounter with a diagnosis of a rickettsial disease in the first or second diagnostic position. An individual could be counted once per lifetime for each type of rickettsial disease. Individuals diagnosed as a case before the start of the surveillance period were excluded. Confirmed cases were prioritized over possible and suspected cases, respectively (Table 2).
These data indicate that a continued multidisciplinary focus on preventive measures to counter the threat of these diseases is warranted. Most important are effective vector control and adherence to personal protective measures.
References
- O'Donnell FL, Stahlman S, Fan M. Surveillance for vector-borne diseases among active and reserve component service members, U.S. Armed Forces, 2010–2016. MSMR. 2018;25(2):8–15.
- Defense Health Agency. Armed Forces Health Surveillance Branch. Armed Forces Reportable Medical Events. Guidelines and Case Definitions, 2017. https://health.mil/reference-Center/Publications/2017/07/17/Armed-Forces-Reportable-Medical-Events-Guidelines. Accessed 17 July 2019.