 Army Capt. Kelly Spencer, a brigade nurse and the officer-in-charge of the 82-bed minimal care ward at the Seattle Event Center in downtown Seattle, Wash., checks her email at the nurse’s station last April. Email is one or many ways to communicate your message to a large audience (Photo by: Army Sgt. 1st Class Brent C. Powell).
Army Capt. Kelly Spencer, a brigade nurse and the officer-in-charge of the 82-bed minimal care ward at the Seattle Event Center in downtown Seattle, Wash., checks her email at the nurse’s station last April. Email is one or many ways to communicate your message to a large audience (Photo by: Army Sgt. 1st Class Brent C. Powell).
Speak early. You will lose momentum if you allow disinformation to supersede your truthful, accurate information. When there is a service, program or process change, use every means available to get the word out immediately across all media platforms. Send out a press release, share it on your sites, create a short video message, set up a hotline, leverage a text message service, or push notifications on your app. Many organizations have created a COVID-19-specific section of their internal and external sites to lessen confusion about where to find official information.
Pushing out information quickly can be challenging due to required coordination. In this case, explain the need for a quick turnaround and stress the importance of passing on critical information as soon as possible. We have ample evidence that patients would rather hear about changes related to their health care from their hospital or clinic vs. a media outlet.
- Quickly getting out accurate information will build trust with your audiences.
Speak often. It’s just not enough to send one email out to staff or to make one social media post regarding an important topic, particularly in regard to COVID-19. We have all learned in our basic communication classes that in any presentation you tell them what you’re going to tell them, you tell them, and then you tell them what you told them! You can’t over communicate health care information and you can’t assume everyone uses your social media platform for their information! Use a variety of mediums frequently to pass information. If you don’t want to clutter up email boxes, create a single daily or weekly news update and push that out instead. Keep it concise and relevant. Remember, you have staff who may not work at computers or have time to wade through pages of information.
Once you post information, don’t walk away. Respond in a timely way, especially on your social media platforms. People are hungry for information and don’t want to wait three days for a response. At Brooke Army Medical Center, we recently hosted a Facebook Live Town Hall about the COVID-19 vaccine program and did our best to answer every question—and there were hundreds! Many were repetitive or had been covered in the Town Hall, but we answered them anyway. Your timely responses help to show the public your organization truly cares.
- People are hungry for information, so be sure to over-communicate.
Speak with accuracy and transparency. Always be transparent and as accurate as possible in your communications, whether speaking with the media or one of your stakeholders. If you can’t discuss details – whether due to HIPAA, operational security or propriety information – don’t dodge the question. Rather, explain WHY there are information restrictions. The reality is, if you don’t tell your story someone else will, and it might not be an accurate depiction. Nothing will destroy trust quicker than a lack of honesty and transparency.
Over the summer, as SARS-CoV-2 virus infection rates skyrocketed, the staff and leadership at BAMC we were questioned about our ability to accept non-military beneficiaries who had COVID-19 into our hospital. By law, we’re not able to do for all. The public perception was that the hospital was sitting out the pandemic – in turn, this affected staff morale. In truth, there were a multitude of ways we were helping to ease the stress on the community health care system. Instead of dodging the questions, we explained the requirements under the law and then offered additional information about the other support we were providing our community.
- If you say nothing, you are allowing someone else to share their perspective of what you are doing - without your voice being heard.
Speak with empathy. The pandemic has underscored the importance of empathy in communication, particularly within the health care system. Frontline health care workers are exhausted and overworked; patients are facing unprecedented uncertainty and fear; and family members are having to suffer through illnesses, alone. It’s more important than ever to express empathy for what they are going through, not in a self-serving way to garner donations or praise, but with sincerity and a true sense of understanding.
Messages need to begin with empathy for the concerns that patients or staff might have and end with another positive message of concern, whether it be for their quality, safe care or their wellbeing as a health care worker. It’s called the peanut-butter sandwich. In the middle, you nest the accurate, transparent information you must share. We received several heartfelt notes and emails about how caring our staff was during a difficult time and shared them in the commander’s weekly message accompanied by a message of gratitude.
- Whether speaking or writing to your staff, patients, or your community, ensure you are sharing a message of compassion, empathy and hope.
One message, many voices. It’s difficult, particularly in larger organizations, to ensure messaging is consistent and accurate. By the time news leaves the Command suite or Front Office, it’s as if a game of telephone kicks in and a much different version reaches the frontline workers. Emails and text messages will only go so far. While communicators can assist with talking points and posts to media platforms, leaders must also use the most successful means of communication—word-of-mouth. Often, this is the most effective means to proliferate the messaging throughout the ranks— pass on news via email and reinforce during team huddles and rounding.
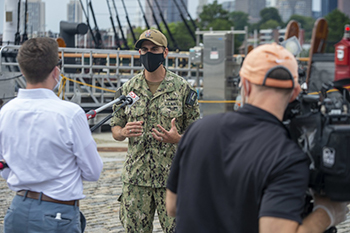 Local media interviews provide an effective means to communicate your message to a broad audience – beyond just your base or military medical treatment facility (Photo by: Navy Seaman Alfonso Ortiz-Lopez).
Local media interviews provide an effective means to communicate your message to a broad audience – beyond just your base or military medical treatment facility (Photo by: Navy Seaman Alfonso Ortiz-Lopez).
As communicators, it’s our duty to maintain consistency across our various platforms. And when the rumors and different perspectives pop up, we must all be ready to transform into myth busters. Equip your internal and external audiences with multiple avenues to ask questions to dispel rumors, whether a hotline, email or open-door policies. When we launched the vaccine program, misperceptions and rumors – from DNA-altering ingredients to live virus inclusion – were spreading as quickly as the virus. To help mitigate rumors, we launched an email program in which staff can ask an infectious disease physician any question and are using them in a Frequently Asked Question document on our internal and external sites.
- Face-to-face communication is often the most effective way to get out your message, and dispel rumors.
Finally, I’d like to emphasize the importance of teamwork. Communication teams have been in high demand over the past year. Lean on your teammates and take time off to rest and recharge. If you’re in a one-person shop, seek out help from your higher headquarters to arrange some much-needed down time. They often can monitor your social media if they have administrative rights. Alternatively, invite hobbyists who can pitch in with taking photos or writing copy in their spare time. I’ve had a few incredible high school and college interns who were thrilled to help out, whether it was for the experience or the credits. I benefited from their social media savvy and fresh outlook, and they benefited with published work they can feature in a portfolio. Definitely a win-win.
In the midst of this public health crisis, we can either keep doing business as usual or use this opportunity to improve and innovate. I’ve been incredibly impressed at what has been accomplished so far in medicine and technology and hope we can apply this same innovative spirit to our internal and external communication. To start, take some time to think about how you have or can improve communication in your organization, and please share your ideas with your public affairs and communication colleagues. I look forward to hearing your success stories and lessons learned.
Elaine Sanchez is a seasoned communications professional with more than 24 years in communications, and currently serves as the Communications Division Chief at the Brooke Army Medical Center in San Antonio, Texas. BAMC is the one of the Department of Defense's largest facilities with a staff of more than 8,000 dedicated soldiers, sailors, airmen, civilians and contractors supporting a 425-bed Academic Medical Center and the DOD’s only Level 1 Trauma Center.