DHA Centers of Excellence collaborate to improve TBI care
 Elizabeth Kirkpatrick, the physical therapist for the Fort Drum Traumatic Brain Injury Clinic at Fort Drum, New York, uses a model of the inner ear to show how a concussion can lead to dizziness and other problems. (Photo by Warren Wright Jr., Fort Drum MEDDAC.)
Elizabeth Kirkpatrick, the physical therapist for the Fort Drum Traumatic Brain Injury Clinic at Fort Drum, New York, uses a model of the inner ear to show how a concussion can lead to dizziness and other problems. (Photo by Warren Wright Jr., Fort Drum MEDDAC.)
When a rocket-propelled grenade struck her helicopter in Afghanistan in 2011, Army Staff Sgt. Beth King sustained a traumatic brain injury and was later diagnosed with post-traumatic stress disorder. Following the event, she experienced headaches, difficulty concentrating, and problems moving around.
King’s story in the A Head for the Future video series shares how she overcame balance issues and learned to pedal a recumbent bicycle and went on to win a gold medal in cycling at the 2019 Warrior Games.
King’s story illustrates the critical role collaboration plays among the Defense Health Agency’s centers of excellence in improving recovery from a traumatic brain injury (TBI).
“Patients often have comorbid conditions such as headache, vertigo, dizziness, and visual disturbances. The joint efforts of the TBI, Psychological Health, Vision, and Hearing Centers of Excellence allow us to cover all aspects of care and management with these unique cases,” said Gary McKinney, chief of clinical practice and clinical recommendations at the Traumatic Brain Injury Center of Excellence (TBICoE) in Silver Spring, Maryland. The centers of excellence are divisions of the Defense Health Agency Research and Development Directorate.
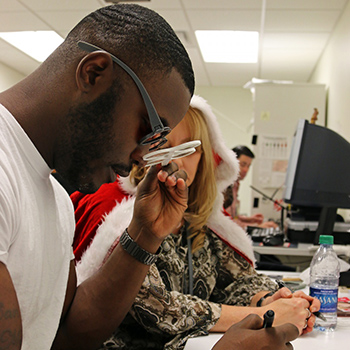 A TBI patient at the Intrepid Spirit Center on Fort Bragg, North Carolina, uses colored glasses as part of vision rehabilitation, Dec. 15, 2017. (Photo by Army Sgt. Paige Behringer.)
A TBI patient at the Intrepid Spirit Center on Fort Bragg, North Carolina, uses colored glasses as part of vision rehabilitation, Dec. 15, 2017. (Photo by Army Sgt. Paige Behringer.)
Dizziness, for example, touches the work being done at several DHA centers of excellence, as damage to different parts of the brain or vestibular system in the inner ear can affect balance, vision and hearing.
According to one study, vestibular complaints were reported by half of TBI patients five years after injury. In 2018, TBICoE revised its clinical screening tool, now called the Military Acute Concussion Evaluation 2, to aid in assessing balance. Recently, TBICoE began revising its 2012 recommendation on dizziness, in collaboration with both the vision and hearing centers. The earlier recommendation was also a collaborative endeavor, based on the results of a 2011 conference consensus.
Vision problems related to TBI also provide opportunities to collaborate.
“It has been estimated that between 43% and 75% of people experiencing TBI events will also experience some form of vision dysfunction, which is why it is beneficial to have eye care professionals assess vision in patients who are involved in a TBI event,” said Dr. Michael Pattison, an optometrist and program manager at the Vision Center of Excellence (VCE). TBICoE participated in developing VCE’s clinical recommendations for treating vision dysfunction in TBI patients. TBICoE staff, including Division Chief Navy Capt. (Dr.) Scott Pyne, served on VCE’s working group, along with vision specialists and other subject matter experts.
TBICoE also worked closely with DHA’s Psychological Health Center of Excellence (PHCoE) to address TBI and PTSD for military health care providers. TBICoE produced a research review on these often co-occurring conditions.
Pattison also pointed out how collaboration contributed to DHA’s mission of satisfied patients and mission readiness.
“With these centers of excellence working together, we can utilize our biggest strengths, the variety of perspectives and experiences we all possess, to provide those that we are entrusted to take care of with the best possible solutions for assisting them to return to full duty and their highest quality of life,” he added. “It has to be a collaborative team approach to meet that mission.”