Abstract
The MSMR has been publishing the results of surveillance studies of malaria since 1995. The standard MSMR case definition uses Medical Event Reports and records of hospitalizations in counting cases of malaria. This report summarizes the performance of the standard MSMR case definition in estimating incident cases of malaria from 2015 through 2017. Also explored was the potential surveillance value of including outpatient encounters with diagnoses of malaria or positive laboratory tests for malaria in the case definition. The study corroborated the relative accuracy of the MSMR case definition in estimating malaria incidence and provided the basis for updating the case definition in 2019 to include positive laboratory tests for malaria antigen within 30 days of an outpatient diagnosis.
What Are the New Findings?
The MSMR case definition provides an estimate of the incidence of malaria in the U.S. Armed Forces. This case definition was updated to include an outpatient health care encounter associated with a laboratory test that is positive for malaria parasite antigen.
What Is the Impact on Readiness and Force Health Protection?
Careful diagnostic evaluation, documentation of confirmed diagnoses, and submission of Medical Event Reports for malaria are crucial for surveillance of the health of the force. Targeted surveillance of special operations forces, members of the Reserve/National Guard, and those stationed in OCONUS embassies would improve DOD malaria risk estimates.
Background
Surveillance for the occurrence of cases of malaria among members of the U.S. Armed Forces has been historically important for many reasons. During World War II, the Korean and Vietnam conflicts, and more recent combat operations in Afghanistan and Somalia, service in regions endemic for malaria was associated with a high incidence of malaria. During World War II, even service at military bases in the southeastern U.S. carried a risk for malaria. Today, the threat of malaria is most apparent for those serving in Korea, Afghanistan, and Africa, but risk also applies for many other regions where transmission still occurs. Surveillance for malaria cases is intended to generate actionable information, in other words, information useful in making policy and command decisions to carry out actions to reduce or eliminate the threat of the disease and the associated morbidity and mortality among service members. For malaria, there are many possible preventive measures, including controlling mosquito vectors (e.g., through the identification and elimination of mosquito breeding sites, as well as the use of pesticides, netting, and repellants on clothing and exposed skin) and using antimicrobial agents to kill infective Plasmodia through chemoprophylaxis and treatment of human malaria infections. In addition, surveillance can provide information about the efficacy of such actions and the extent to which they are being carried out.
The MSMR has published the results of surveillance studies of malaria cases in service members since 1995.1 Initial studies counted mainly the Medical Event Reports (MERs) of cases of malaria submitted through the Reportable Medical Events System (RMES) for conditions deemed notifiable because of their public health importance. In 2002, the MSMR added diagnoses of malaria made during hospitalizations to its surveillance case definition.2 Diagnoses from hospitalizations were counted only if they were recorded in the first diagnostic position of the record of hospitalization. In the Jan. 2011 annual MSMR update on malaria cases, a more detailed case definition was used for the first time. The most noteworthy change in the new case definition was the addition of cases from some hospitalization records in which the diagnosis of malaria was not in the first diagnostic position.3 The details of that case definition are described in the Methods section.
The Jan. 2012 MSMR presented the results of an analysis of sources of variability in estimates of malaria case counts. Counts of MERs of malaria, hospitalizations with diagnoses of malaria, and outpatient encounters with diagnoses of malaria were examined. Additional factors considered were diagnoses that listed a particular species of Plasmodium, patient histories of travel to malarious countries, and laboratory tests ordered and found positive for malaria. The findings of that analysis prompted no changes to the MSMR criteria for cases of malaria.4
This report describes an analysis that re-examined the MSMR criteria for counting cases of malaria as well as other possible surveillance criteria for identifying cases among members of the U.S. Armed Forces. The goal of the analysis was to evaluate the use of current and possibly revised criteria in arriving at surveillance estimates for the incidence of malaria. Surveillance diagnoses of malaria based upon administrative and public health records lack complete clinical information that would permit validation of apparent cases and exclusion of misdiagnoses. A potential misclassification bias in malaria surveillance data could limit the application of findings toward public health action.
This study performed an assessment of the validity of data sources used in malaria surveillance, including inpatient and outpatient records and MERs. The goal was a better understanding of the over- and under-estimation of malaria cases and how misclassification would impact confidence in the estimates of the true burden of malaria disease. Also explored in this analysis were factors that may affect the under- or over-reporting of malaria, such as service in special operations, in the reserve and National Guard, during deployment, and overseas.
Methods
The surveillance period was 1 Jan. 2015 through 31 Dec. 2017. The surveillance population included all individuals who served in an active or reserve component of the U.S. Army, Navy, Air Force, or Marine Corps at any time during the surveillance period.
The MSMR case definition for a case of malaria used in annual updates for years 2010 through 2017 specified that a case is defined as an individual with documentation of 1 of the following: 1) an MER record of confirmed malaria, 2) a hospitalization record with a diagnosis of malaria in the first (primary) diagnostic position, 3) a hospitalization record with a non-primary diagnosis of malaria due to a specific Plasmodium species, 4) a hospitalization record with a non-primary diagnosis of malaria plus a diagnosis of anemia, thrombocytopenia and related conditions, or malaria complicating pregnancy in any diagnostic position, or 5) a hospitalization record with a non-primary diagnosis of malaria plus diagnoses of signs or symptoms consistent with malaria (as listed in the Control of Communicable Diseases Manual, 18th Edition) in each diagnostic position antecedent to malaria.5 The relevant ICD-9 and ICD-10 codes are shown in the first table of the annual update for 2018 (pages 2–7 of this issue).6 This analysis allowed 1 case of malaria per service member per 365-day period. When multiple records documented a single episode, the date of the earliest encounter was considered the date of clinical onset, and the most specific diagnosis was used to classify the Plasmodium species.
To identify additional malaria cases that did not meet the MSMR case definition, further review of inpatient, outpatient, RMES, and laboratory data was performed. The standardized records of the Defense Medical Surveillance System (DMSS) were searched for all records of inpatient and outpatient health care encounters for which a diagnosis of malaria was documented. DMSS records of MERs of notifiable cases of malaria were also captured. All MERs that reported malaria were examined whether the diagnosis was described as "confirmed" or not (e.g., unconfirmed, suspect, possible, or pending).
Malaria diagnoses that were recorded only in the records of outpatient encounters (i.e., not hospitalized or reported as a notifiable event) have not been considered case-defining in previous analyses because of concerns with poor predictive value. In this analysis, such encounters were examined to assess the possibility that true cases of malaria might be overlooked among individuals with only outpatient diagnoses of malaria. The Navy and Marine Corps Public Health Center (NMCPHC) provided records of all laboratory tests for malaria that were positive during the surveillance period. The NMCPHC identified positive and suspect cases of malaria by querying the Composite Health Care System Health Level 7 (HL7) chemistry and microbiology laboratory databases for records that contained the terms "plasmodium" or "malaria". Positive laboratory tests included microscopic identification of plasmodium on thin and thick smears and plasmodium positive antigen rapid diagnostic tests. Malaria antibody tests were excluded. Only positive test results were included. Individuals with negative laboratory test results could not be distinguished from individuals who had not been tested. Such positive tests were linked to the records of health care encounters (both inpatient and outpatient) and of MERs. In an attempt to validate the identification of malaria cases using the MSMR case definition, the clinical records of a subset of cases and non-cases were reviewed using the electronic health records in the Armed Forces Health Longitudinal Technology Application (AHLTA).
Random samples of 25 malaria cases that met the MSMR case definition and of 25 individuals whose records did not meet the case definition were selected. Individuals who did not meet the MSMR case definition included those whose only malaria diagnoses were in the records of outpatient encounters, those whose only malaria diagnosis was recorded in an unconfirmed MER, or those whose hospitalization diagnoses of malaria did not meet the case definition criteria. Cases were validated by reviewing military electronic outpatient and inpatient records, with an emphasis on laboratory confirmation, provider evaluation and assessment, and medications consistent with a malaria diagnosis. There were 4 additional patients for whom medical records did not have sufficient information because of hospitalization at non-military facilities. Those patients were contacted directly to obtain the additional records needed to confirm case status. Correction factors obtained from these samples were applied to the total population of individuals who had at least 1 outpatient encounter, 1 hospitalization, or 1 MER with a diagnosis of malaria to obtain weighted estimates of the true burden of malaria.7 The false positive and false negative cases were closely examined for factors potentially related to misclassification, such as service in overseas deployed locations, in the National Guard or Reserve, or in special operations assignments. When applied, exact confidence intervals were used because of small sample sizes.
Results
During the 3-year surveillance period, there were 1,028 instances in which a diagnosis of malaria was recorded in a record of an MER (n=121), an inpatient encounter (n=82), or an outpatient encounter (n=825). A total of 319 unique service members accounted for these diagnoses.
Malaria cases based on the MSMR case definition
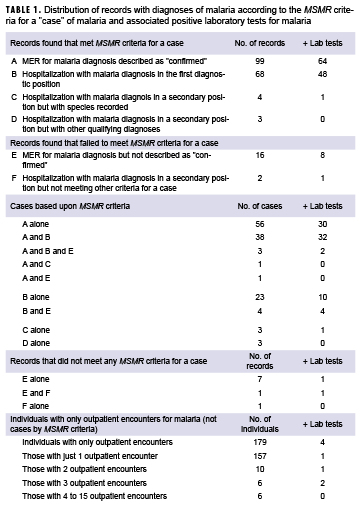
A total of 132 cases of malaria, among 131 unique individuals, were identified using the MSMR case definition. (One service member had separate diagnoses of malaria 21 months apart.) Of the 132 cases, 99 qualified as cases on the basis of a "confirmed" MER and 75 on the basis of a hospitalization that met the criteria for a case. Many cases (n=42) met the case definition criteria on the basis of both a confirmed MER and a hospitalization, but 57 cases were based upon only a confirmed MER and 33 cases were based upon only a hospitalization (Table 1).
MERs
Of the 121 MERs submitted for a diagnosis of malaria, 105 of them were characterized as "confirmed" diagnoses. Six of the 105 were duplicate reports for episodes of illness already reported via MERs, so there were 99 MER cases of malaria among 98 individuals. Of the 121 MERs submitted, 16 did not characterize the diagnosis of malaria as confirmed. However, 8 of those individuals otherwise met the MSMR case definition for malaria by virtue of a separate "confirmed" MER (n=4), a record of hospitalization that met the criteria for a case (n=7), or both (n=3) (Table 1).
Hospitalizations
Among the 82 hospitalizations associated with recorded diagnoses of malaria, 2 did not meet any of the MSMR criteria for a hospitalized case of malaria. Of the remaining 80 hospitalizations, 73 had the diagnoses recorded in the first diagnostic position, but 5 of those hospitalizations were repeat hospitalizations within 365 days of a prior such hospitalization, so there were 68 cases that met the case criteria based upon the first diagnostic position. For the 7 hospitalized cases with malaria diagnoses not in the first diagnostic position, 4 met the case definition by virtue of a species-specific diagnosis for malaria, and the records of 3 cases included accompanying diagnoses indicative of malaria. A total of 75 hospitalizations met the case definition criteria for cases of malaria (Table 1).
Outpatient encounters with diagnoses of malaria
Of the 319 unique individuals associated with malaria diagnoses in records of inpatient or outpatient encounters or MERs, 291 service members had at least 1 outpatient encounter with a recorded diagnosis of malaria, and 28 service members had no outpatient encounters with diagnoses of malaria. Of the 132 cases that met the MSMR case definition for malaria (among 131 individuals), 111 cases had at least 1 outpatient encounter with a recorded diagnosis of malaria, and 21 cases had no associated outpatient malaria diagnoses. Of the 188 service members who did not meet the MSMR case definition for malaria, 181 had at least 1 outpatient encounter with a recorded diagnosis of malaria and 7 had no outpatient diagnoses of malaria.
Among those 179 service members who had only outpatient diagnoses of malaria and thus did not meet the MSMR case definition for malaria, 22 had more than 1 such encounter and 157 had only a single outpatient encounter (Table 1).
Positive laboratory tests for malaria
The NMCPHC identified 503 positive laboratory tests for malaria during the period. Those positive results were associated with 88 distinct service members, 78 of whom had records that met the MSMR case-defining criteria for malaria (79 cases) and 10 of whom had no such case-defining diagnosis.
Laboratory results among cases
Among the 99 cases of malaria associated with an MER of confirmed malaria, 64 had a positive laboratory test and 35 did not. Among the 75 cases of malaria associated with a hospitalization that met the MSMR criteria for a malaria case, 49 had a positive laboratory test and 26 did not. Among the 42 cases that met both the MER and hospitalization MSMR criteria for a malaria case, 34 cases had positive laboratory results and 8 did not (Table 1).
Laboratory results among non-cases
Among the 9 service members who did not meet the MSMR criteria on the basis of a non-confirmed diagnosis of malaria in an MER (n=8), a hospitalization that did not meet the criteria (n=2), or both (n=1), 2 had positive laboratory tests (for plasmodial antigen) and 7 did not. The service member with a positive laboratory test who failed to meet both criteria was hospitalized for severe trauma; malaria was the eighth diagnosis listed in the hospitalization record. The other service member in this category was reported as a "confirmed" case of malaria in an MER. The individual had a positive laboratory test during pre-deployment screening for blood banking purposes, but it was determined that the result was highly likely a false positive based upon lack of symptoms and having grown up in Africa. The service member was not treated for malaria.
Laboratory results among individuals who had only outpatient encounters
Of the 179 service members whose only malaria diagnoses were found in the records of outpatient encounters, 22 individuals had more than 1 outpatient encounter. Three of the 22 were found to have at least 1 positive laboratory test for P. falciparum antigen. One of these service members had 2 outpatient encounters 2 days apart in Germany. The first encounter listed only the diagnosis for falciparum malaria, and the second encounter included only the codes for falciparum malaria and for personal history of malaria. Chart review indicated that the service member had been evacuated from a deployment in Africa, but there were no documented hospitalizations or MERs for this individual. The other 2 service members with positive laboratory results each had 3 outpatient encounters at Fort Bliss, TX, for which the records listed falciparum malaria and unspecified malaria as diagnoses. The encounters for the 2 service members were during Jan. to March 2015 and July to Aug. 2015, respectively. Chart reviews indicated that, coincidentally, the initial outpatient encounters for each took place about 2 weeks after return from a visit to families in Cameroon. Again, there were no documented hospitalizations or MERs for either individual. Among the 157 service members with a single outpatient encounter, just 1 was found to have a positive laboratory test but it was not an antigen test. Clinical assessment concluded that it was probably a false positive smear test in an individual who did not have a travel history compatible with a risk of acquiring malaria.
Review of clinical records of selected cases and possible cases
In an attempt to validate the identification of malaria cases using the MSMR case definition, the clinical records of a subset of cases and non-cases were reviewed using the electronic records in AHLTA. Of particular interest were the findings in the records of some of the individuals who had only outpatient records of malaria diagnoses. Three of the 4 outpatient records with associated positive laboratory tests for malaria appeared to represent true cases of malaria based upon positive tests for malaria antigen, more than 1 outpatient diagnosis of malaria, and encounter records describing circumstances highly indicative of clinical malaria. The records for the fourth possible case indicated that the laboratory test was not an antigen test and the clinical assessment included information that made a diagnosis of malaria seem unlikely.
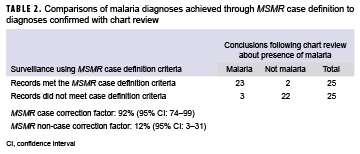
Additional clinical records were reviewed for random samples of 25 service members who met the MSMR case definition criteria for malaria and 25 who did not meet the case definition but who had some documentation for malaria indicated by outpatient or inpatient diagnoses, laboratory tests, or unconfirmed MERs. Two of the 25 surveillance cases of malaria could not be validated as cases by chart reviews. Three of the 25 individuals whose records did not satisfy the criteria of the MSMR case definition were judged to be true malaria cases on the basis of chart reviews (Table 2).
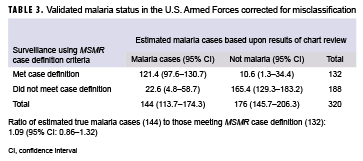
In the sample, the correction factors were 92% (23/25) and 12% (3/25) (Table 2). These are the proportion of MSMR case definition identified cases that would be assigned as cases based on chart review and the proportion of non-MSMR case definition identified cases that would be assigned as cases based on chart review, respectively. After applying the correction factors to the total number of malaria cases observed among those that met (n=132) and did not meet (n=188) the MSMR case criteria during the surveillance period, the estimated true number of cases was calculated to be 144 (Table 3). This was 9% higher than the number of cases (n=132) identified when using the MSMR case definition.
Of the 22 individuals who were true negative cases, 13 (59%) had malaria diagnoses recorded during health care encounters prior to travel to malarious areas, 5 (23%) had symptoms of other pathology or were ruled out for malaria, and the clinical records of 4 (18%) had no corroborating evidence of a malaria diagnosis or of malaria treatment in outpatient or inpatient records.
Of the 23 true positive cases, 17 (74%) had a positive laboratory test in electronic medical records. All of the other 6 had plausible exposures to malarious areas. Two were diagnosed while deployed, 1 to Afghanistan and 1 to Djibouti, and both cases had a physician note stating that a positive test result had been obtained. One was clinically assessed as malaria and was treated presumptively before laboratory testing was performed. Two had physician notes from civilian medical facilities stating that testing had been performed and that the diagnosis was confirmed. There were 5 who contracted malaria while visiting friends and relatives overseas. One was a soldier who had been assigned to an embassy in Africa, and his records were only available through direct patient contact. The locations of presumed malaria transmission were Africa (14, including 2 exclusively in Djibouti), Korea (5), and Afghanistan (4). There were 10 documented cases of P. falciparum, 4 with P. vivax, and 9 that were unspecified. There were 7 treated with artemeter/lumefantrine, 8 with atovaquone/proguanil, 2 with chloroquine (P. vivax cases only), 1 with artesunate, and 5 with unspecified treatment.
Among the 2 false positive cases, there was 1 Army National Guardsman and 1 Navy Reservist. The Army soldier had already been discharged from the National Guard 3 months prior to diagnosis. Among the false negative cases, there were 2 special operations service members and 1 soldier who had recently returned from Embassy service in Africa. All 3 had sought care in civilian medical treatment facilities.
Editorial Comment
The analysis indicated that the use of MERs and hospitalization records were reasonable approaches to estimating the incidence of cases of malaria among service members. Diagnoses of malaria documented in MERs or in records of hospitalizations were the result of careful evaluations of incident illnesses. This report shows that after accounting for misclassification, the estimated number of true malaria cases between 2015 and 2017 was 144 (95% CI: 126–162), which was very close to the MSMR case definition estimate of 132. Most of the correctly classified non-cases were associated with pre-travel outpatient visits during which malaria prophylaxis was given. Among the small number of misclassified true cases of malaria, all had a history of service either in special operations, an overseas embassy, or the National Guard or Reserve component. All of the false negatives had been hospitalized at a civilian medical treatment facility. Of particular interest was the observation that, although outpatient encounters with recorded diagnoses of malaria alone did not add greatly to the total numbers of cases, the association of such outpatient encounters with contemporaneous positive laboratory tests for malaria did appear to identify a few additional cases of malaria during the surveillance period. For this reason, the MSMR case definition has been modified to add a category of case defined by a positive laboratory test for malaria antigen in an individual who had a record of an outpatient diagnosis of malaria within 30 days of the specimen collection date.
The submission through the Disease Reporting System Internet (DRSi) of an MER of a reportable condition such as malaria is dependent upon the investigation by local public health authorities of possible cases occurring within their area of responsibility.8 In the case of malaria, preparation of an MER would require not only knowledge of a specific individual with an illness whose signs and symptoms are compatible with malaria, but also knowledge of the results of laboratory tests that confirm the diagnosis. Collection of such information presumes that the public health official has gathered such information from medical staff caring for the individual, the laboratory, and the ailing individual (for information about relevant travel and deployment history and use of chemoprophylaxis). Given the need for such information to justify the submission of an MER, it is reasonable to presume that an MER reporting a confirmed case of malaria represents credible surveillance information.
Because of the above description of the information that would warrant the submission of an MER of confirmed malaria through DRSi, it would seem reasonable that there should be additional documentation in the Military Health System (MHS) electronic databases of 1 or more of the following for each MER confirmed case: a hospitalization record that lists a diagnosis of malaria, a record of an outpatient encounter that lists a malaria diagnosis, a positive laboratory test for malaria; or pharmacy documentation of treatment with anti-malarial medications. Such additional documentation would be most expected for cases that were diagnosed at fixed military medical facilities where local surveillance by public health personnel would collect the information needed to justify an MER of confirmed malaria.
For diagnoses of malaria reported by an MER from non-fixed military medical facilities, such as those in deployment settings, where the documentation of health care encounters and of laboratory test results may be less than complete, documentation in electronic databases may not adequately reflect all cases of malaria. Lack of confirmatory information may not only reduce the frequency with which local public health personnel can confirm true cases of malaria, but may also handicap the ability of centralized surveillance agencies like the Armed Forces Health Surveillance Branch (AFHSB) to ascertain cases.
Most, if not all, hospitalizations associated with a diagnosis of malaria met the detailed criteria of the MSMR case definition. Because hospitalization records in the DMSS contain discharge diagnoses, there is an underlying presumption that these diagnoses were recorded after initial diagnostic uncertainties had been resolved. Although tentative diagnoses of malaria may be considered by health care providers at the time of admission to hospital, the diagnosis is unlikely to appear in the list of final diagnoses unless the evaluation of the patient's illness and the patient's response to treatment for malaria are compatible with that diagnosis.
Another factor affecting the completeness of documentation of malaria cases is the provision of purchased health care to service members in civilian treatment facilities. Although the MHS receives documentation of such care that includes diagnoses such as malaria, the results of laboratory testing and the documentation of malaria treatment are often not available. Moreover, civilian health care providers do not prepare or submit MERs for reportable conditions such as malaria. For service members who are diagnosed and treated for malaria in the civilian health care setting, the preparation and transmission of an MER depends upon the initiative of the local military public health authorities. Moreover, service members treated for malaria by civilians in an outpatient setting might never be recognized as cases without efforts by military public health officials to collect the results of the relevant laboratory testing as the basis for submitting an MER of a confirmed case.
The use of records of outpatient encounters alone to define cases of malaria has not been adopted in the AFHSB case definition of malaria because of a variety of considerations. First, provisional or tentative diagnoses of malaria are often entered into outpatient records while the results of laboratory tests for malaria are pending. One previous analysis found that documentation of malaria laboratory test performance was infrequent for those with only outpatient diagnoses of malaria and that none of the laboratory tests performed was positive for malaria.4 Second, miscoding of diagnoses of malaria may occur in conjunction with health care encounters for prescribing malaria chemoprophylaxis or provision of malaria prevention counseling. Lastly, inadvertent, erroneous use of malaria codes in encounter records may occur. Prior analysis has found a very low likelihood that a patient with only an outpatient diagnosis of malaria actually has malaria.4
The review of a subset of clinical records for individuals who did and did not meet the MSMR criteria for malaria cases was informative. As described above, outpatient diagnoses of malaria in association with positive tests for malaria antigen found in laboratory data did not meet the criteria for the existing MSMR case definition but were assessed as true malaria cases by chart review. For this reason, the MSMR has decided to add this group to the case definition. However, the small proportion of additional malaria cases (12%) found among the randomly selected individuals who did not meet the MSMR case definition (most of whom were found in outpatient data only) does not appear to justify further change to the case definition. While their inclusion would slightly increase the identification of malaria cases, it would also result in the inclusion of a large number of false positive cases.
The MSMR case definition used in this and previous issues of the MSMR closely matched the estimate of the true burden of malaria in the U.S. military obtained from chart review.6 The lower estimates used by the Centers for Disease Control and Prevention in their surveillance reports reflect a strict case definition requiring lab confirmation by blood smear or polymerase chain reaction, which likely underestimates the true disease burden.9
The main limitation of this report is the absence of a true "gold standard" for malaria case status. The chart review adds additional information, getting closer to such a standard, but some of the records may have been incomplete, leading to persistent misclassification. Such misclassification is likely to lead to an underestimate of malaria since the likelihood of misclassification is greater in the cases not meeting the case definition because of incomplete records. However, this study demonstrates that the magnitude of this residual error is likely to be small.
This study suggests that the U.S. military should have confidence that the MSMR estimates are close to the true burden of malaria disease and that the impact and trends identified by surveillance are accurate. However, it also suggests that selected populations, including special operations, Reserve/National Guard, and those stationed in overseas embassies, should be targeted for increased active surveillance. Moreover, better capture of inpatient hospitalizations at civilian medical facilities is needed to ensure quality of care for the service member, communication of health issues to military providers, and proper surveillance by military public health authorities. Finally, Reportable Medical Events surveillance should be strengthened in order to provide the timeliness, accuracy, and precision needed to inform force health protection policy.
Acknowledgements: The authors thank the Navy and Marine Corps Public Health Center, Portsmouth, VA, for providing laboratory data for this analysis.
References
- U.S. Army Center for Health Promotion and Preventive Medicine. Malaria in active duty soldiers. MSMR. 1995;1(5):8–9.
- U.S. Army Center for Health Promotion and Preventive Medicine. Malaria among active duty soldiers, U.S. Army, 2001. MSMR. 2002;8(3):2–4.
- Armed Forces Health Surveillance Center. Update: Malaria, U.S. Armed Forces, 2010. MSMR. 2011;18(1):2–6.
- Armed Forces Health Surveillance Center. Sources of variability of estimates of malaria case counts, active and reserve components, U.S. Armed Forces. MSMR. 2012;19(1):7–10.
- Armed Forces Health Surveillance Branch. Surveillance Case Definition: Malaria. Dec. 2014. https://health.mil/Reference-Center/Publications/2014/12/01/Malaria.
- Armed Forces Health Surveillance Branch. Update: Malaria, U.S. Armed Forces, 2018. MSMR. 2019;26(2):2–7.
- Fleiss, Joseph L. Statistical Methods for Rates and Proportions. John Wiley & Sons, New York; 1973.
- Armed Forces Health Surveillance Branch [in collaboration with U.S. Air Force School of Aerospace Medicine, Army Public Health Center, and Navy and Marine Corps Public Health Center]. Armed Forces Reportable Medical Events Guidelines and Case Definitions. 17 July 2017.
- Mace KE, Arguin PM, Tan KR. Malaria Surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(7):1–28.