What Are the New Findings?
As in prior years, musculoskeletal disorders, injuries, mental health disorders, and pregnancy-related conditions accounted for relatively large proportions of the morbidity and health care burdens among active component service members. Injuries accounted for the largest percentage of medical encounters and individuals affected, and mental health disorders accounted for the largest number of hospital bed days.
What Is the Impact on Readiness and Force Health Protection?
Injuries, musculoskeletal disorders, and mental health disorders are major detractors from service members’ individual readiness and deployability and can lead to early separation and disability. Reducing their impact on force readiness can be accomplished through enhanced measures to prevent and treat the occurrence of such disorders.
Background
Perceptions of the relative importance of various health conditions in military populations often determine the natures, extents, and priorities for resources applied to primary, secondary, and tertiary prevention activities. However, these perceptions are inherently subjective and may not reflect objective measures of the relationship between the conditions and their impact on health, fitness, military operational effectiveness, health care costs, and so on.
Several classification systems and morbidity measures have been developed to quantify the "public health burdens" that are attributable to various illnesses and injuries in defined populations and settings.1 Not surprisingly, different classification systems and morbidity measures lead to different rankings of illness- and injury-specific public health burdens.2
For example, in a given population and setting, the illnesses and injuries that account for the most hospitalizations are likely different from those that account for the most outpatient medical encounters. The illnesses and injuries that account for the most medical encounters overall may differ from those that affect the most individuals, have the most debilitating or long-lasting effects, and so on.2 Thus, in a given population and setting, the classification system or measure used to quantify condition-specific morbidity burdens shapes to a large extent the conclusions that may be drawn regarding the relative importance of various conditions and, in turn, the resources that may be indicated to prevent or minimize their impacts.
This annual summary uses a standard disease classification system (modified for use among U.S. military members) and several health care burden measures to quantify the impacts of various illnesses and injuries among members of the active component of the U.S. Armed Forces in 2018.
Methods
The surveillance period was 1 Jan. through 31 Dec. 2018. The surveillance population included all individuals who served in the active component of the U.S. Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. All data used in this analysis were derived from records routinely maintained in the Defense Medical Surveillance System (DMSS). These records document both ambulatory encounters and hospitalizations of active component members of the U.S. Armed Forces in fixed military and civilian (if reimbursed through the Military Health System [MHS]) treatment facilities worldwide.
For this analysis, DMSS data for all inpatient and outpatient medical encounters of all active component members during 2018 were summarized according to the primary (first-listed) diagnosis (if reported with an International Classification of Diseases, 10th Revision, Clinical Modification [ICD-10-CM] code between A00 and T88, an ICD-10 code beginning with Z37, or Department of Defense [DOD] unique personal history codes DOD0101–DOD0105). For summary purposes, all illness- and injury-specific diagnoses (as defined by the ICD-10) were grouped into 142 burden of disease-related conditions and 25 categories based on a modified version of the classification system developed for the Global Burden of Disease (GBD) Study.1 In general, the GBD system groups diagnoses with common pathophysiologic or etiologic bases and/or significant international health policymaking importance. In this analysis, some diagnoses that are grouped into single categories in the GBD system (e.g., mental health disorders) were disaggregated to increase the military relevance of the results. Also, injuries were categorized by affected anatomic site rather than by cause because external causes of injuries are incompletely reported in military outpatient records.
The “morbidity burdens” attributable to various “conditions” were estimated based on the total number of medical encounters attributable to each condition (i.e., total hospitalizations and ambulatory visits for the condition with a limit of 1 encounter per individual per condition per day), numbers of service members affected by each condition (i.e., individuals with at least 1 medical encounter for the condition during the year), and total bed days during hospitalizations for each condition.
The new electronic health record for the MHS, MHS GENESIS, was implemented at several military treatment facilities during 2017. Medical data from sites that are using MHS GENESIS are not available in DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounters for individuals seeking care at any of these facilities during 2018 were not included in this analysis.
Results
Morbidity Burden, by Category
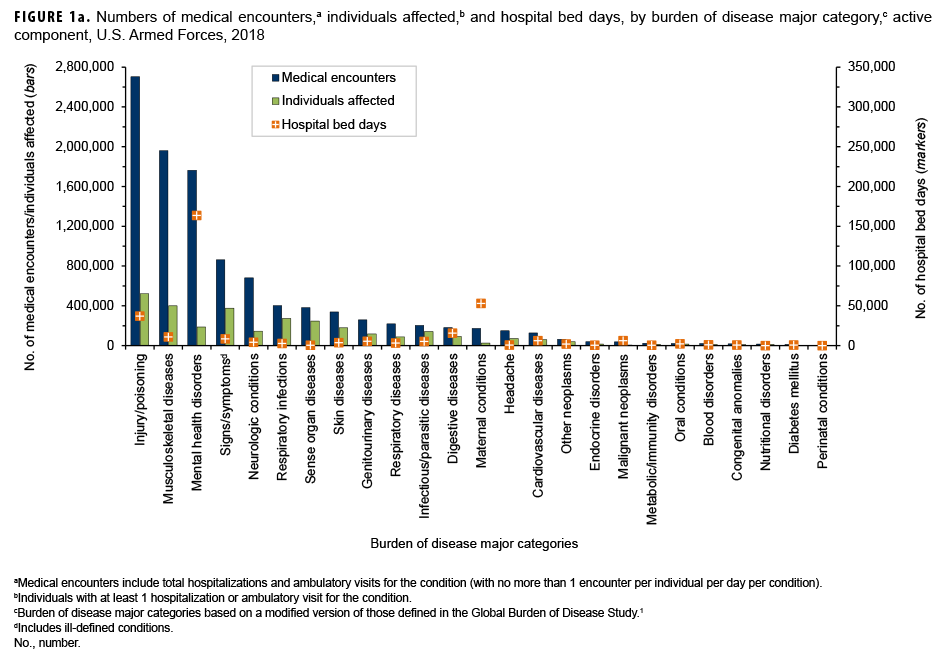
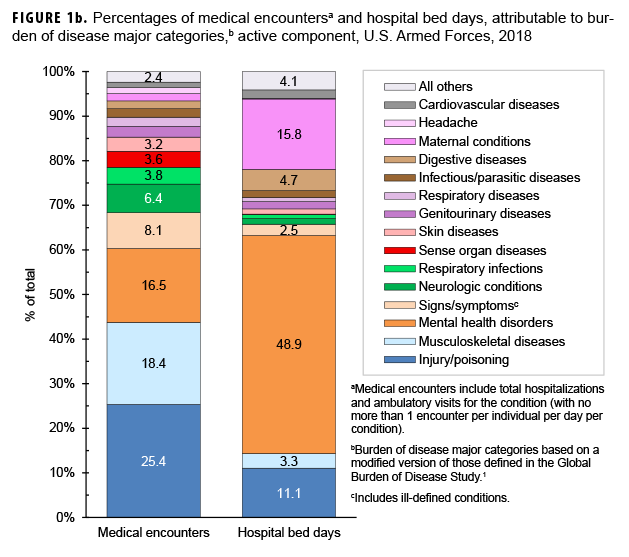
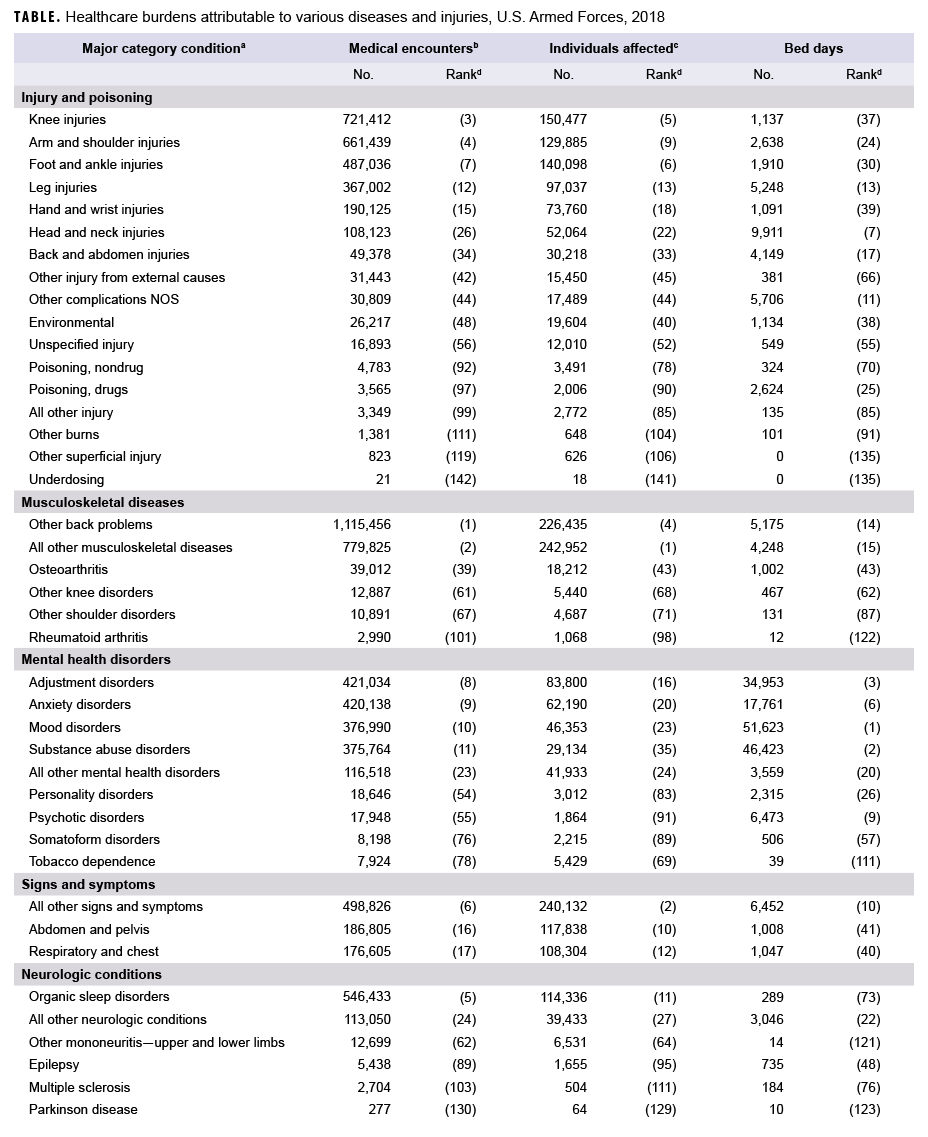
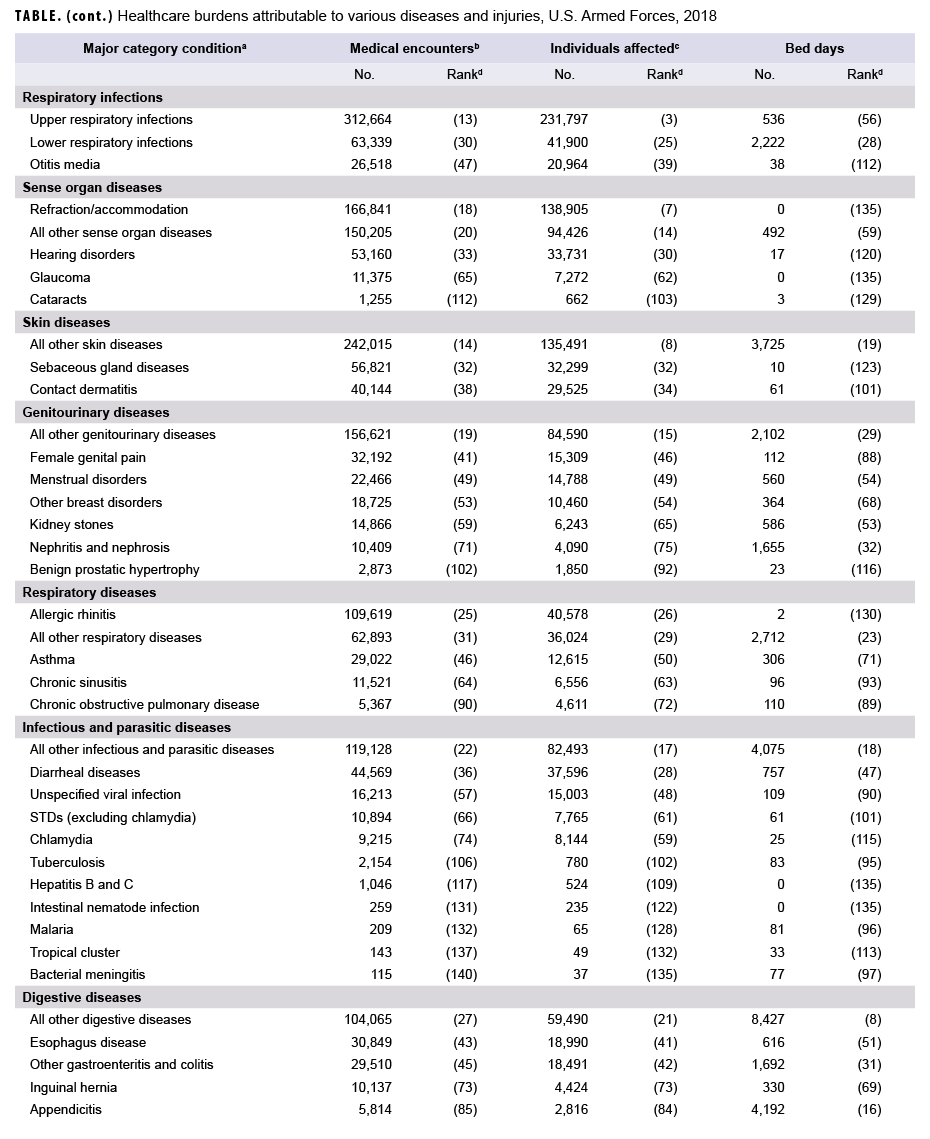
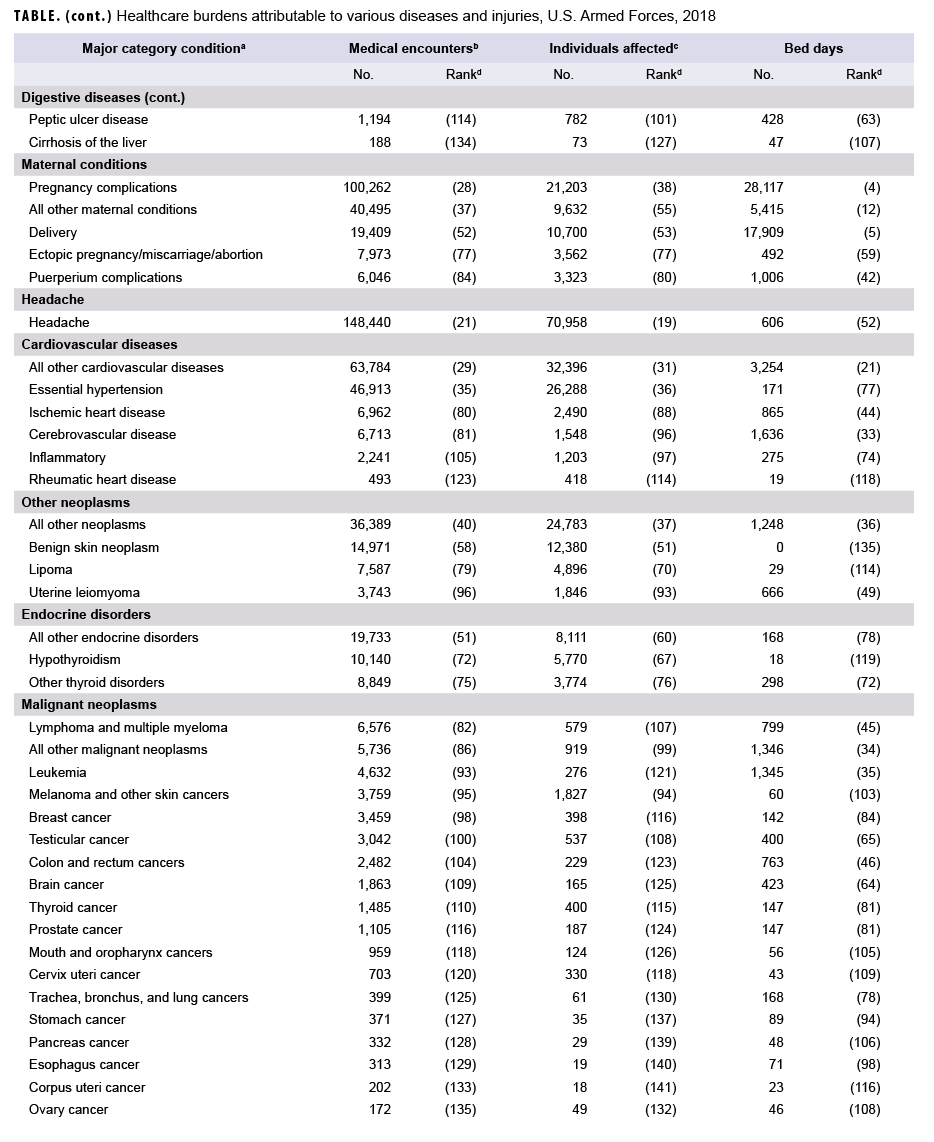
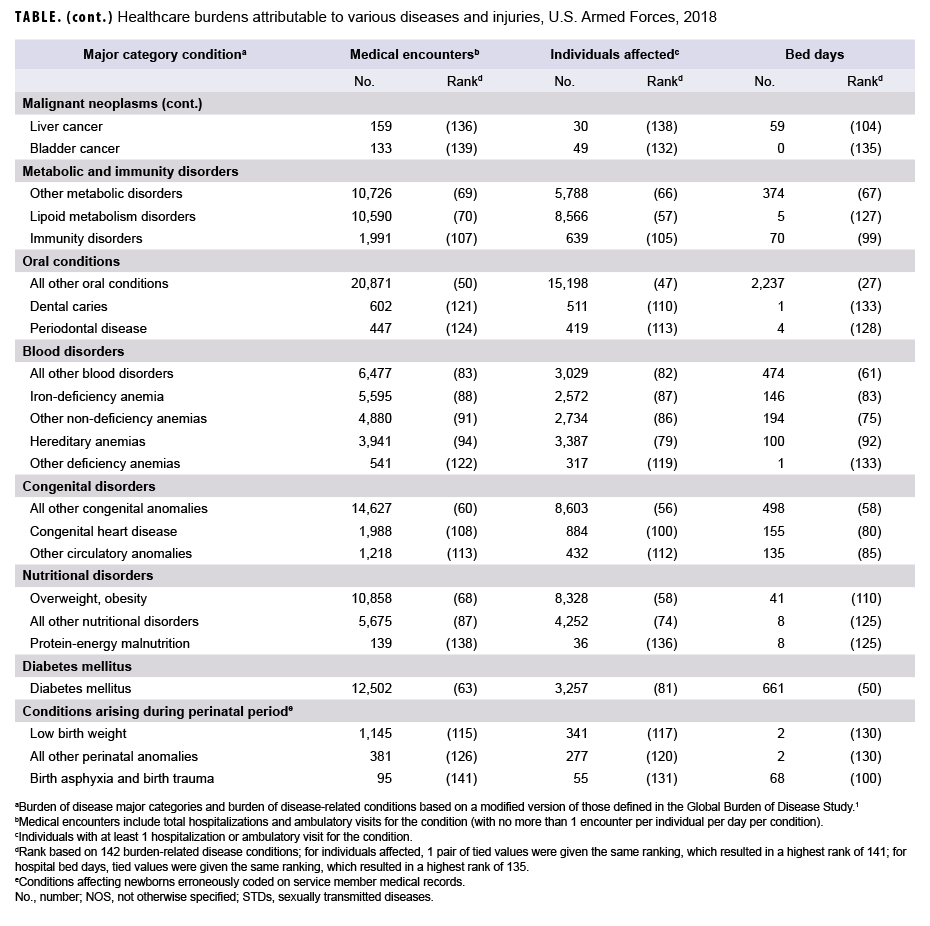
In 2018, more service members (n=522,854) received medical care for injury/poisoning than any other morbidity-related category (Figures 1a, 1b). In addition, injury/poisoning accounted for more medical encounters (n=2,703,799) than any other morbidity category and one-quarter (25.4%) of all medical encounters overall.
Mental health disorders accounted for more hospital bed days (n=163,652) than any other morbidity category and 48.9% of all hospital bed days overall (Figures 1a, 1b). Together, injury/poisoning and mental health disorders accounted for nearly three-fifths (59.9%) of all hospital bed days and more than two-fifths (41.9%) of all medical encounters.
Of note, maternal conditions (including pregnancy complications and delivery) accounted for a relatively large proportion of all hospital bed days (n=52,939; 15.8%) but a much smaller proportion of medical encounters overall (n=174,185; 1.6%) (Figures 1a, 1b). Routine prenatal visits are not included in this summary.
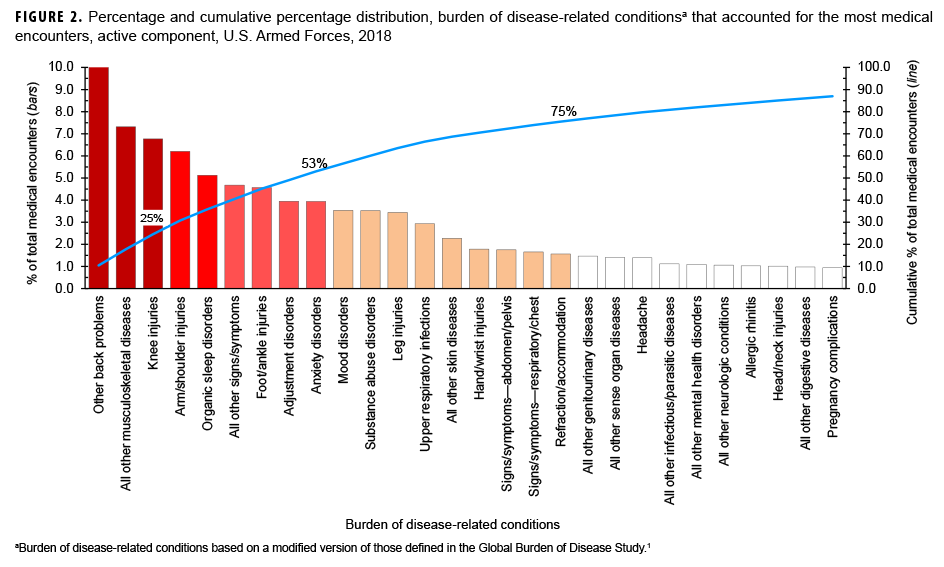
Medical Encounters, by Condition
In 2018, the 3 burden of disease-related conditions that accounted for the most medical encounters (i.e., other back problems, all other musculoskeletal diseases, and knee injuries) accounted for almost one-quarter (24.5%) of all illness- and injury-related medical encounters overall (Figure 2). Moreover, the 9 conditions that accounted for the most medical encounters were responsible for more than half (53.0%) of all illness- and injury-related medical encounters overall. In general, the conditions that accounted for the most medical encounters were predominantly musculoskeletal disorders (e.g., back problems), anatomic site-defined injuries (e.g., injuries of the knee, arm/shoulder, or foot/ankle), and mental health disorders (e.g., adjustment disorders, anxiety disorders, or mood disorders) (Table, Figure 2).
Individuals Affected, by Condition
In 2018, more service members received medical care for "all other musculoskeletal diseases" than for any other specific condition (Table). Of the 10 conditions that affected the most service members, 3 were anatomic site-defined injuries (injuries of the knee, foot/ankle, and arm/shoulder), 2 were musculoskeletal diseases (all other musculoskeletal diseases and other back problems), 2 were signs and symptoms (all other signs and symptoms and abdomen and pelvis), 1 was a respiratory infection-related condition (upper respiratory infections), 1 was a sense organ disease (refraction/accommodation), and 1 was a skin disease-related condition (all other skin diseases).
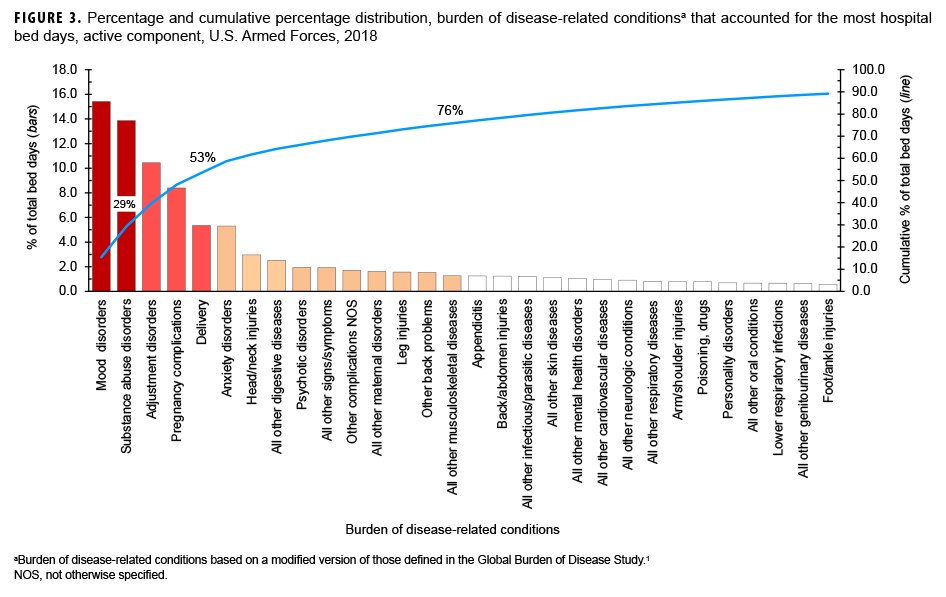
Hospital Bed Days, by Condition
In 2018, mood and substance abuse disorders accounted for more than one-quarter (29.3%) of all hospital bed days. Together, 4 mental health disorders (mood, substance abuse, adjustment, and anxiety) and 2 maternal conditions (pregnancy complications and delivery) accounted for more than half (58.8%) of all hospital bed days (Table, Figure 3). Approximately one-ninth (11.1%) of all hospital bed days were attributable to injuries and poisonings.
Relationships Between Health Care Burden Indicators
There was a strong positive correlation between the number of medical encounters attributable to various conditions and the number of individuals affected by the conditions (r=0.86) (data not shown). For example, the 3 leading causes of medical encounters were among the 5 conditions that affected the most individuals (Table). In contrast, there were weak to moderate positive relationships between the hospital bed days attributable to conditions and either the numbers of individuals affected by (r=0.17) or medical encounters attributable to (r=0.36) the same conditions (data not shown). For example, labor and delivery and substance abuse disorders were among the top-ranking conditions in terms of proportion of total hospital bed days; however, these conditions affected relatively few service members.
Editorial Comment
This report reiterates the major findings of prior annual reports on morbidity and health care burdens among U.S. military members. In particular, this report documents that a majority of the morbidity and health care burdens that affect active component U.S. military members are attributable to just 6.3% of the 142 burden of disease-defining conditions considered in the analysis.
In 2018, as in prior years, musculoskeletal disorders (particularly of the back), injuries (particularly of the knee and arm/shoulder), mental health disorders (particularly adjustment, anxiety, substance abuse, and mood disorders), and pregnancy- and delivery-related conditions accounted for relatively large proportions of the morbidity and health care burdens that affected active component service members. Nine burden of disease-related conditions accounted for slightly more than half of all illness- and injury-related medical encounters of active component members and included 2 mental health disorders (adjustment and anxiety disorders), 3 anatomic site-defined injuries (knee, arm/shoulder, and foot/ankle), 2 musculoskeletal conditions (other back problems and all other musculoskeletal diseases), organic sleep disorders, and all other signs and symptoms.
It should be noted that this annual summary for 2018 was based on the use of ICD-10 codes exclusively. This is the third MSMR burden report that did not use ICD-9 codes. Because of some of the differences between the 2 generations of coding (e.g., compared to ICD-9, ICD-10 has more than 4 times as many codes, often allows for much greater specificity of diagnoses, and has added and deleted some specific diagnoses or terminology), direct comparisons of the counts for 2018 with those from years before 2016 should be interpreted with caution. Dramatic changes in counts and rankings for specific categories or conditions may reflect changes in incidence or prevalence, the effects of a different coding system, the adjustment of health care providers to the new coding system, or combinations of all 3.
Mental health disorders (including substance abuse disorders), injuries, and musculoskeletal disorders of the back have been leading causes of morbidity and disability among service members throughout military history.3–8 It is well recognized that the prevention, treatment, and rehabilitation of back problems and joint injuries, and the detection, characterization, and management of mental health disorders—including substance abuse and deployment stress-related disorders (e.g., post-traumatic stress disorder)—should be the highest priorities for military medical research, public health, and force health protection programs.
In summary, this analysis, like those of prior years, documents that relatively few illnesses and injuries account for most of the morbidity and health care burdens that affect U.S. military members. Illnesses and injuries that disproportionately contribute to morbidity and health care burdens should be high-priority targets for prevention research and resources.
References
- Murray CJL, Lopez AD, eds. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press, 1996:120–122.
- Brundage JF, Johnson KE, Lange JL, Rubertone MV. Comparing the population health impacts of medical conditions using routinely collected health care utilization data: nature and sources of variability. Mil Med. 2006;171(10):937–942.
- Jones BH, Perrotta DM, Canham-Chervak ML, Nee MA, Brundage JF. Injuries in the military: a review and commentary focused on prevention. Am J Prev Med. 2000;18(3 suppl):71–84.
- Ritchie EC, Benedek D, Malone R, Carr-Malone R. Psychiatry and the military: an update. Psychiatr Clin North Am. 2006;29(3):695–707.
- Stahlman S, Oetting AA. Mental health disorders and mental health problems, active component, U.S. Armed Forces, 2007–2016. MSMR. 2018;25(3):2–11.
- Cozza KL, Hales RE. Psychiatry in the Army: a brief historical perspective and current developments. Hosp Community Psychiatry. 1991;42(4):413–418.
- Watanabe HK, Harig PT, Rock NL, Koshes RJ. Alcohol and drug abuse and dependence. In: Jones FD, Sparcino LR, Wilcox VL, Rotherberg JM, eds. Military Psychiatry: Preparing in Peace for War. Part I of Textbook of Military Medicine Series. Washington, DC: Office of the Surgeon General, Department of the Army. Borden Institute; 1994. https://ke.army.mil/bordeninstitute/published_volumes/military_psychiatry/MPch5.pdf. Accessed 2 April 2019.
- Army Medical Surveillance Activity. Relative burdens of selected illnesses and injuries, U.S. Armed Forces, 2001. MSMR. 2002;8(2):24–28.