What are the New Findings?
Incidence of plant dermatitis remained stable between 2010 and 2015, increased in 2016 and 2017, then decreased in 2018 through 2020. The highest rates were seen among male and non-Hispanic White service members, in the younger age groups and among those in combat-related occupations. Most cases occurred in the summer months and at combat training installations.
What is the Impact on Readiness and Force Health Protection?
Plant dermatitis can cause significant disability and lost duty time particularly in highly sensitized individuals. Service members should be informed of the risk of exposure particularly during combat-training, and advised on poisonous plant identification and personal protective measures to prevent exposure.
Abstract
Dermatitis (skin inflammation) caused by the oil of poisonous plants is an occupational hazard for U.S. military members who are assigned and train in endemic areas. Plant dermatitis can cause significant disability, substantial medical costs, and lost duty time. During the 11-year surveillance period there were 73,725 cases of plant dermatitis diagnosed in active component service members (rate: 5.3 per 1,000 person-years [p-yrs]). The overall incidence rates remained relatively stable between 2010 and 2015, increased in 2016 and 2017, then decreased in 2018 through 2020. Compared to their respective counterparts, incidence rates were highest among male service members (5.7 per 1,000 p-yrs), the youngest (<20 years) service members (8.4 per 1,000 p-yrs), non-Hispanic White service members (7.5 per 1,000 p-yrs), members of the Army (7.7 per 1,000 p-yrs) and Marine Corps (6.5 per 1,000 p-yrs), and among those in combat-related occupations (11.9 per 1,000 p-yrs). More than half of the cases occurred during summer months and about one-third of all cases were diagnosed at 4 installations: Fort Benning, Georgia (n=11,257); Camp Pendleton, CA (n=5,399); Fort Bragg, NC (n=4,259), and Fort Campbell, KY (n=3,221). Service members, particularly young individuals in combat-training in endemic states, should be informed of the risks associated with exposures to toxic plants and advised on personal protective measures.
Background
Plant dermatitis is an allergic inflammatory skin reaction in response to the oils of poisonous plants. In the U.S., the most common dermatitis-causing plant genus is Toxicodendron (formerly Rhus) (i.e., poison ivy, poison oak, and poison sumac).1 Approximately 50%–75% of the U.S. adult population are susceptible to skin reactions upon exposure to Toxicodendron oil or oleoresin, called urushiol. In these sensitized individuals, responses to the oils at the sites of exposure produce intense redness and pruritus (itch); severe cases can result in edema, fluid-filled vesicles or bullae, and extreme discomfort. Plant dermatitis is generally self-resolving and lasts approximately 3 weeks; however, symptoms can persist up to 6 weeks in highly susceptible individuals.1
Toxicodendron species are indigenous to the United States and flourish in forests, fields, wetlands, road sides, parks, and backyards. Poisonous plants are an occupational hazard for U.S. military members who are assigned to and train in endemic areas. Plant dermatitis can cause significant disability as well as result in substantial medical costs and lost duty time. This report describes the numbers and incidence rates of plant dermatitis in active component service members, its seasonality, and its distribution across U.S. military installations during 2010–2020.
Methods
The surveillance period was from Jan. 1, 2010 to Dec. 31, 2020. The surveillance population included all individuals who served in the active component of the Army, Navy, Air Force, or Marine Corps at any time during this period. For this analysis, the Defense Medical Surveillance System (DMSS) was searched for records of inpatient and outpatient care for diagnoses of plant dermatitis. A case was defined by the recording of 1 inpatient or outpatient diagnosis of plant dermatitis (International Classification of Diseases, 9th Revision Clinical Modification [ICD-9-CM]: 692.6; ICD-10-CM: L23.7, L24.7, L25.5) in any diagnostic position; an individual could be an incident case once every 30 days. Diagnoses were also derived from records of medical encounters of deployed service members documented in the Theater Medical Data Store (TMDS), which is incorporated into the DMSS.
Results
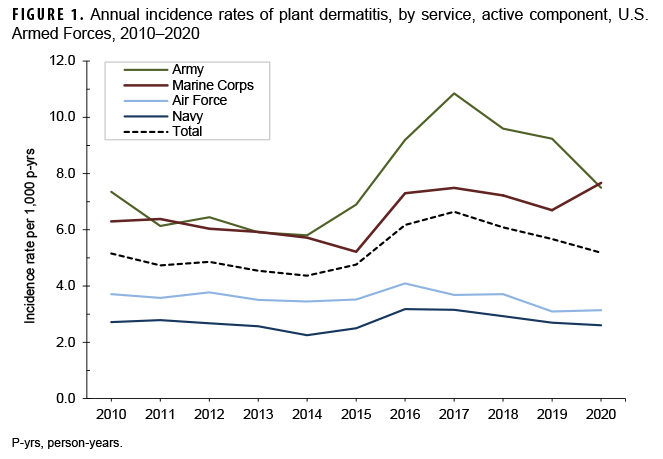
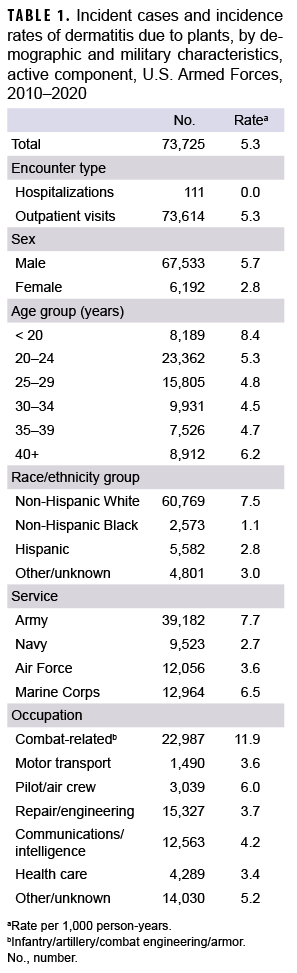
During the surveillance period, there were 73,725 diagnoses of plant dermatitis (crude incidence rate: 5.3 per 1,000 person-years [p-yrs]) (Table 1). Most of the cases (99.9%) were diagnosed in outpatient facilities; 111 service members had hospitalizations with a case-defining diagnosis for plant dermatitis. Sixty-four hospitalizations (57.7%) had a case-defining diagnosis in the first or second diagnostic position compared to 98.0% of outpatient encounters (data not shown). Overall incidence rates remained relatively stable between 2010 and 2015, increased in 2016 and 2017, then decreased in 2018 through 2020 (Figure 1). The highest annual rate was in 2017 (6.6 per 1,000 p-yrs).
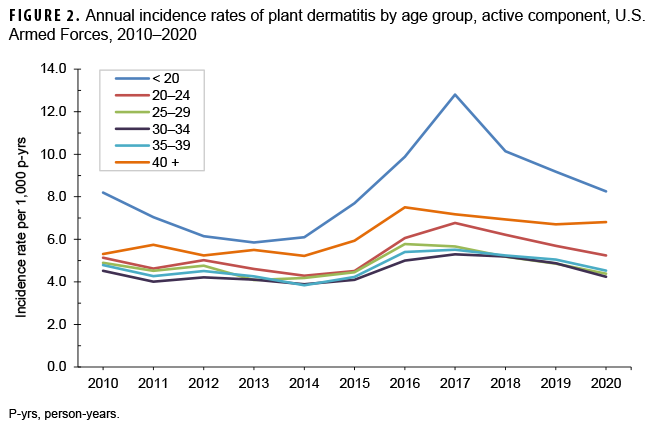
Compared to their respective counterparts, incidence rates of plant dermatitis were higher among male service members (5.7 per 1,000 p-yrs) and in the youngest (<20) and oldest (40+) service members (8.4 and 6.2 per 1,000 p-yrs, respectively) (Table 1). The annual incidence rates among those under age 20 were highest during the period 2016–2020 (Figure 2). Incidence rates among non-Hispanic White service members (7.5 per 1,000 p-yrs) were more than 6 times those among non-Hispanic Black service members (1.1 per 1,000 p-yrs). Rates were also higher among members of the Army and Marine Corps (7.7 and 6.5 per 1,000 p-yrs, respectively) compared to their respective counterparts. The increases in the rates of plant dermatitis from 2015 through 2017 were driven by increases in the Army and Marine Corps; rates in the Air Force and Navy remained comparatively low and stable (Figure 1). Of note, in 2020, the rate of plant dermatitis among Marine Corps members exceeded that of the Army for the first time since 2011.
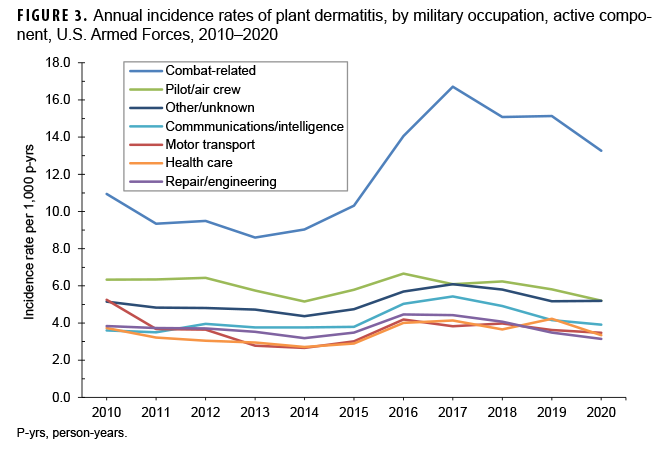
The incidence rate among those in combat-related occupations (11.9 per 1,000 p-yrs) was almost double the rate among the next highest occupational rate, pilot/air crew (6.0 per 1,000 p-yrs) (Table 1). The rates in combat-related occupations remained consistently higher than other military occupations; there was a notable increase in incidence rates from 2015 (6.8 per 1,000 p-yrs) to a high in 2017 (16.7 per 1,000 p-yrs) (Figure 3).
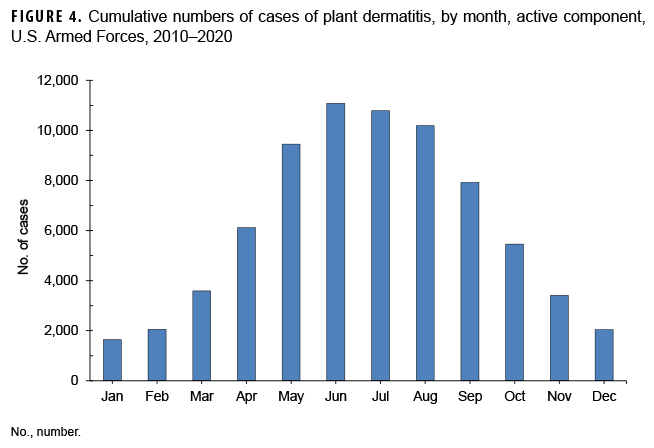
There was distinct seasonality to plant dermatitis incidence; more than two-thirds of the cumulative cases (67%) occurred during the 5 months of May to September (Figure 4). More cases were diagnosed among service members serving in Georgia (n=12,874), California (n=8,764), North Carolina (n=7,707) and Virginia (n=7,125) than any other states (data not shown). While numbers of cases in California, North Carolina, and Virginia remained relatively stable during the period, cases in Georgia increased steadily from a low of 659 in 2013 to a high of 1,885 in 2017 (data not shown). Of all military installations in the U.S. with cases, nearly one-third of all cases were diagnosed at 4 installations: Fort Benning, GA (n=11,257); Camp Pendleton, CA (n=5,399); Fort Bragg, NC (n=4,259), and Fort Campbell, KY (n=3,221) (data not shown).
During the 11-year surveillance period, a total of 107 service members received a plant dermatitis diagnoses while deployed (data not shown). Most cases were among soldiers, male and non-Hispanic White service members, service members aged 20–29, and those in repair/engineering occupations (data not shown). Almost three-quarters (71.0%) of cases occurred during the 5 months of May to September (data not shown).
Editorial Comment
The crude incidence rates of plant dermatitis increased approximately 27% from 2010 to the peak annual incidence rate in 2017. This change was driven by increases among service members in the Army and Marine Corps (data not shown), among those in combat-specific occupations, and among those under age 20. Furthermore, plant dermatitis cases were most numerous among those serving at installations that support extensive ground combat training in Georgia, California, and North Carolina. The relatively high rates among the youngest (and most junior and inexperienced) service members may be related to their relatively frequent and intensive exposures to field conditions during recruit and subsequent occupation-specific training.
It is estimated that 50% to 75% of U.S. adults are clinically sensitive to Toxicodendron species.1 This report documented that crude incidence rates of plant dermatitis were nearly 7 times higher among non-Hispanic White than non-Hispanic Black service members. This finding should be interpreted cautiously because the analysis did not account for potentially confounding differences between race/ethnicity groups of service members (e.g., occupational/leisure time activities, medical care seeking behaviors). There are no other studies or surveillance reports that confirm or indicate that there are strong demographic correlates of susceptibility to Toxicodendron species.
In light of the geographic distributions of Toxicodendron species in the U.S., cases in Georgia, North Carolina, and Virginia are most likely attributable to Eastern poison ivy, while cases in California are most likely due to poison oak.2 Not surprisingly, summer months pose the greatest risk of exposure; however, plant dermatitis affects U.S. military members throughout the year and in every U.S. state as well as abroad. To some extent, plant dermatitis incidence may be related to weather patterns; for example, moderate drought tends to increase the growth of Toxicodendron species. During drought conditions, water sensitive trees, shrubs, and plants may be overrun by Toxicodendron species which are invasive and opportunistic.4,5 Toxicodendron species have been shown to outgrow other woody species and produce more potent urushiol under higher levels of CO2.5 A previous MSMR article demonstrated an increase in cases of plant dermatitis at Fort Benning following reported drought conditions.6 From 2014 through 2016, Georgia experienced moderate to extreme drought conditions followed by an overabundance of rain in 2017.7,8 It is plausible that the dramatic increase in cases from 2014 and peak in 2017 may have been driven by the specific drought conditions in the state of Georgia causing an increase in poison ivy growth.
Although small in number, plant dermatitis cases do occur during deployment. In addition to animal and insect threats, service members should be advised of potential poisonous plant species that occur in foreign locations.
There are several limitations to this report that should be considered when interpreting the results. Cases presenting for care in health care facilities may represent more severe cases where the individuals were more motivated to seek treatment. Minor cases of poison ivy are most likely underreported as individuals may self-treat and not seek care. Additionally, it cannot be determined the extent to which cases may be exposed and acquire plant dermatitis during non-military activities (e.g., hiking, camping, lawn care).
In this report, hospitalized cases may include individuals who were not explicitly hospitalized for plant dermatitis. Approximately one-third of hospitalizations (n=35) had a case-defining code in the primary diagnostic position; an additional 29 cases (26.1%) and 19 cases (17.1%) had a case-defining code in the second and third diagnostic position, respectively (data not shown). Future studies may consider refining the case definition for hospitalizations to be more restrictive and thus more likely to capture true hospitalizations for plant dermatitis.
Military members, particularly those in ground combat units, should be informed of the risks associated with exposures to toxic plants and personal protective measures. For example, awareness and concern should be heightened during summer months, particularly during/after periods of drought. Proper identification and avoidance of Toxicodendron plants, and use of protective clothing are effective preventive measures against plant dermatitis.
Author Affiliations: Defense Health Agency, Armed Force Health Surveillance Branch (Ms. Daniele and Dr. Taubman).
References
- Gladman AC. Toxicodendron dermatitis: poison ivy, oak, and sumac. Wilderness Environ Med. 2006;17(2):120–128.
- NIOSH Workplace Safety and Health Topics: Poisonous plants. Centers for Disease Control. Accessed July 20, 2011. https://www.cdc.gov/niosh/topics/plants/
- National Oceanic and Atmospheric Administration, National Climatic Data Center: Historical Palmer Drought Indices. Accessed 20 July 2011. https://www.ncdc.noaa.gov/temp-and-precip/drought/historical-palmers/
- Dickinson CC, Jelesko JG, Barney JN. Habitat Suitability and Establishment Limitations of a Problematic Liana. Plants (Basel). 2021;10(2):263.
- Schnitzer SA, Londré RA, Klironomos J, Reich PB. Biomass and toxicity responses of poison ivy (Toxicodendron radicans) to elevated atmospheric CO2: comment. Ecology. 2008;89(2):581–585.
- Armed Forces Health Surveillance Center. Plant dermatitis, active component, 2001–2010. MSMR. 2011;18(7):19–21.
- Pendered D. Georgia drought free, suffering from overabundance of rain. Saporta Report. Published August 11, 2017. Accessed 14 October 2021. https://saportareport.com/georgia-drought-free-suffering-overabundance-rain/sections/reports/david/
- United States Department of Agriculture. 2016 Drought Map. Accessed 14 Oct. 2021. https://www.nrcs.usda.gov/wps/portal/nrcs/detail/ga/technical/dma/?cid=nrcseprd1301268