Abstract
An outbreak of SARS CoV-2 infection occurred in an infantry battalion from Joint Base Lewis-McChord following participation in a field training exercise in the vicinity of Yakima, WA in February of 2021. Extreme weather during the exercise disrupted planned COVID-19 mitigation measures and caused 110 soldiers to be sheltered in a small aircraft hangar for several nights. The probable index case reported to sick call with symptoms compatible with COVID-19, but the soldier was not diagnosed with COVID-19, was returned to duty, and was allowed to remain in the enclosed hangar for 3 additional days. In total, 143 individuals with epidemiologic ties to the field training exercise tested positive for SARS-CoV-2 during the outbreak. Nine samples sent for sequencing were determined to be the SARS-CoV-2 Beta variant. This report illustrates important lessons learned whose implementation in the future will enable better protection of service members from COVID-19 and similar health risks associated with training.
What Are the New Findings?
COVID-19 is a threat to military exercises because of the virus's ability to cause illness in a large number of soldiers. Results of this investigation demonstrate the potential impact of a COVID-19 outbreak in land-based military congregate living settings, especially those with shared sleeping spaces.
What Is the Impact on Readiness and Force Health Protection?
In addition to immunization, pre-deployment screening, basic hygiene measures such as sufficient sleeping space, and ready access to appropriate clinical assessment and diagnostic testing can be important parts of mitigating the risk of a potential COVID-19 outbreak in military training settings.
Background
This report describes an outbreak of SARS-CoV-2, the causative agent of COVID-19, that peaked during Feb. 21–26, 2021 and was tied to a single military training event. A total of 143 laboratory-confirmed cases were identified. Nine samples collected within the first several days of the outbreak (Feb. 20–23, 2021) were sent for sequencing upon noting an increase in the baseline SARS-CoV-2 positivity rate among individuals in a congregate setting. All 9 samples were determined to be the SARS-CoV-2 variant B.1351, referred to by the World Health Organization naming scheme as the Beta variant.
The first case of SARS-CoV-2 infection known to be caused by the Beta variant (501Y.V2/B.1.351 lineage) was reported in South Africa on Dec. 18, 2020.1 The Beta variant was first reported in the U.S. in South Carolina on Jan. 28, 2021.2 By March 23, 2021, the Washington State Department of Health had reported 8 cases while the Centers for Disease Control (CDC) had reported 219 cases of Beta variant in 27 jurisdictions nationally.3,4 Similar to the Alpha (B.1.1.7) variant first reported in December 2020, the Beta variant has been linked to higher viral load and increased transmissibility compared to other SARS-CoV-2 variants that were identified at the time.5 Other known attributes of the variant include moderate reduction in neutralization by monoclonal antibody therapeutics, convalescent sera, and post-vaccination sera.6 Additionally, clinical trial data have also shown a decreased efficacy of some coronavirus disease 2019 (COVID-19) vaccines primarily due to antigenic changes in the SARS-CoV-2 spike protein.7,8 To date, there is no evidence suggesting that the Beta variant is associated with an increase in disease severity.9,10
This report aims to describe the setting, timeline, and characteristics of an outbreak of COVID-19 Beta variant among an infantry battalion from Joint Base Lewis-McChord (JBLM), WA following participation in a field training exercise at a local Army training center in Yakima, WA in February 2021.
Methods
Population and setting
During Feb. 4–19, 2021, an Infantry Battalion (herein Battalion A) of a Brigade (herein Brigade X) from JBLM conducted a tactical field training exercise at an Army training center in Yakima, WA. Brigade X is an infantry unit comprised of 8 battalions; battalions typically consist of about 1,000 soldiers distributed among 4 to 6 companies. Neither symptom-based nor laboratory-based COVID-19 screening of the soldier participants was performed prior to deployment. Soldiers of Battalion A conducted platoon- and company-level training in groups of approximately 40 or 275 personnel at a time rotating through different training iterations to maximize physical distance between soldiers as much as practically possible. Hand washing stations were placed near all tactical operations centers, latrines, and designated dining areas. Use of face covering was mandated by policy and enforced by leadership. Despite COVID-19 mitigation measures that were integrated in the planning of the field training exercise, extreme environmental conditions and logistical difficulties made these measures difficult to execute and maintain.
On Feb. 12, 2021, the training center experienced extreme weather with temperatures reaching 13 °F (-10 °C) with roughly 2 inches (5 cm) of snow and wind gusts up to 14 mph. Because of these conditions, 110 soldiers (an infantry company of 103 soldiers and a group of 7 medics from a separate supporting company) were moved into a relatively small aircraft hangar on the night of Feb. 12, 2021, for protection from freezing temperatures; this was the sleeping arrangement for the remainder of the field training exercise. The aircraft hangar was approximately 75 ft (23 m) x 85 ft (26m) or 6,375 square feet (592 square meters) in size (Figures 1, 2). The hangar had no mechanical heating or ventilation system and the windows were kept closed to keep the heat in. Furthermore, because of limited space, many soldiers slept on the ground in their military issued 5-component modular sleep systems with roughly 2 feet of space between soldiers. Based on minimum acceptable sleeping space allowance of 72 square feet of floor space per person,11 the aircraft hangar had a maximum capacity of 88 personnel (6,375/72=88.5). By housing 110 soldiers in this space, the unit's use of the hangar exceeded recommended public health capacity by 22 soldiers.
The unit returned earlier than planned to JBLM on Feb. 18–19, 2021, using buses within which recommended physical distancing could not be achieved. Shortly after returning to JBLM, a small number of soldiers began reporting symptoms of COVID-19. On Feb. 20, 2021, the Battalion physician assistant was notified of what was later identified as the index case of this outbreak; the case had tested positive for SARS-CoV-2 earlier the same day. The affected soldier reported initial symptoms of fever (101.6 °F, 38.7 °C) and chills that started on Feb. 16, 2021. This soldier was evaluated by medics in the field on the day of his symptom onset but was not suspected as having COVID-19. The soldier was rehydrated and was promptly returned to duty where he resumed normal training activities for the next 3 days among other soldiers, including sleeping in the enclosed hangar. When the presence of an outbreak was confirmed, representative respiratory samples were collected and sent for sequencing; these samples were from cases that were among the first diagnosed and most highly connected to other cases.
Case identification
All cases identified (service members and beneficiaries) were diagnosed using PCR testing through Madigan Army Medical Center's laboratory. Case interview and contact tracing were performed for all individuals with laboratory-confirmed COVID-19 infection by the unit medical section with assistance from JBLM Department of Public Health. Close contact was defined using CDC's criteria of being within 6 feet of someone with laboratory-confirmed SARS-CoV-2 infection for a cumulative total of 15 minutes or more over a 24-hour period during the window of high-risk viral transmission (2 days prior to symptom onset or if asymptomatic, prior to a positive test, until completion of the isolation period). Contact tracing included civilian close contacts. Genome sequencing for variants was completed on an Illumina MiSeq (Illumina, San Diego, CA) at U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID).
Results
Outbreak investigation
The index case described above was the first symptomatic soldier from the hangar to test positive for COVID-19. Identification of this case triggered immediate contact tracing by the Battalion medical section which resulted in 21 individuals being quarantined for close contact with the index case. On Feb. 21, 2021, the day after the first laboratory-confirmed case was reported, 2 additional individuals tested positive for SARS-CoV-2 COVID-19 (Figure 3). Although these 2 individuals were not identified as close contacts by the index case as they worked in different sections, they were found to have slept in the same enclosed hangar during the field training exercise. The identification of these cases triggered the quarantine and testing of 7 additional soldiers. By the end of the day on Feb. 21, a total of 18 individuals had tested positive for COVID-19 from Battalion A. Contact tracing for the first 3 positive cases revealed a total of 28 individuals (including civilians and beneficiaries) as close contacts who were subsequently quarantined and tested. By 24 February 2021, 46 individuals from the infantry company had tested positive for COVID-19. At this point the remainder of the company was placed into quarantine and tested.
Following several iterations of contact tracing, the total number of positive cases from this company reached 87. Forty-two additional positive cases were identified in the support company to which the medical detachment belonged. These 2 companies accounted for 129 (90.8%) of the 142 positive cases in Battalion A from Feb. 21 to March 4, 2021. An additional 19 cases were identified as part of this outbreak that were not part of the battalion, but were linked epidemiologically. As above, 9 samples from the outbreak were sent for sequencing, all of which were determined to be SARS-CoV-2 Beta variant.
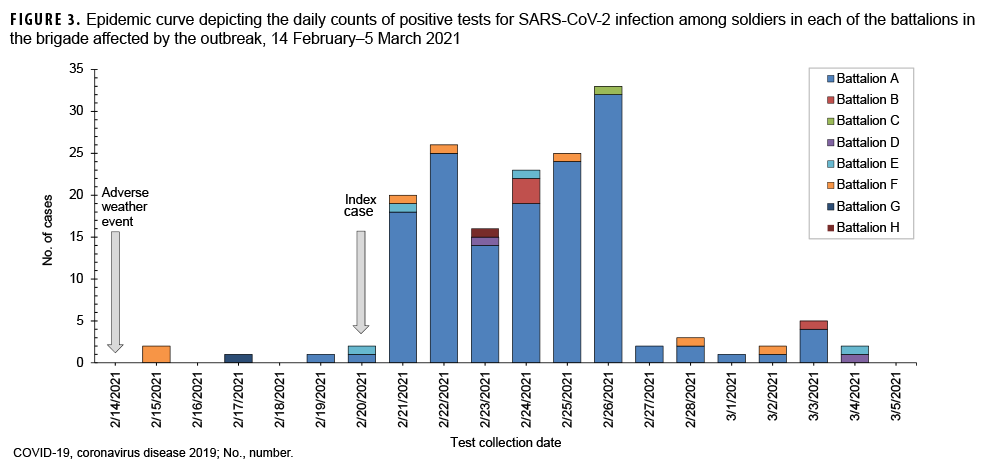
The distribution of daily counts of positive tests for SARS-CoV-2 infection among soldiers in each of the battalions represents an outbreak from Feb. 14, 2021 to March 5, 2021 (Figure 3). Cases from Battalion A caused a sudden and dramatic increase of daily COVID-19 cases in Brigade X beginning Feb. 21, 2021 and ending Feb. 26, 2021, clearly marking the beginning and end of the peak outbreak period. The index case was not included in the peak outbreak period as this soldier tested positive on Feb. 20. Of note, it is likely that many of the cases identified in the first few days of the outbreak may have become infected earlier. Battalion A accounted for 92.3% (132/143) of the cases during this period, and the daily average of COVID-19 cases during the peak outbreak period was 24. Comparatively, the daily average of COVID-19 cases during the 7 days preceding the outbreak (Feb. 14–20, 2021, the pre-outbreak period) was less than 1. In the late-outbreak period (Feb. 27–March 5, 2021), the average daily COVID-19 case count decreased to 2, a 91.7% decrease compared to the peak outbreak period.
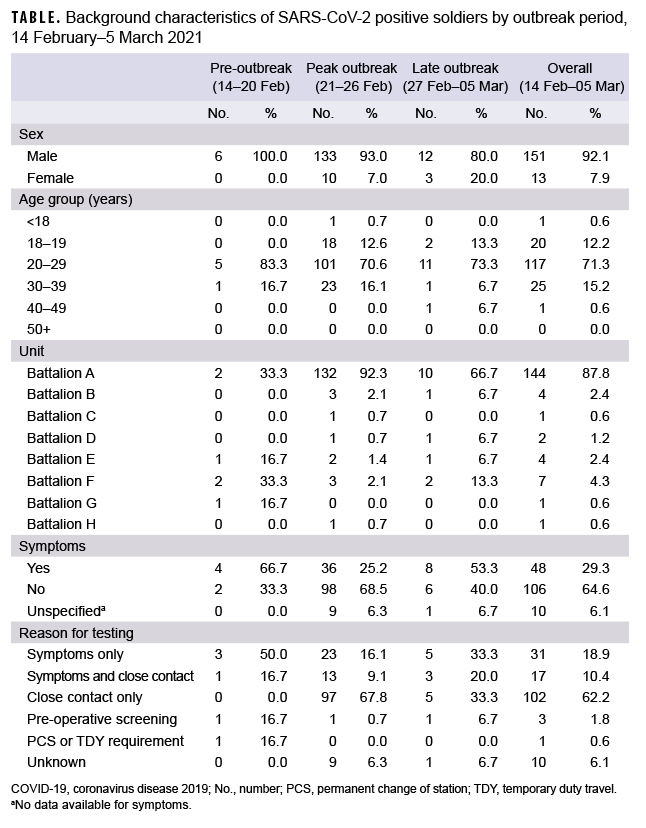
The distribution of COVID-19 cases before, during, and after the peak period of the outbreak reflect the age distribution of the infantry units involved, the concentration of cases in Battalion A, and the high proportion of infected soldiers who were asymptomatic but were identified through methodical contact tracing (Table). In total, 164 individuals from the study cohort sample tested positive for SARS-CoV-2 from Feb. 14 through March 5, 2021. The field training exercise (FTX) was held from Feb. 9–19, 2021. The majority of samples tested were collected in the days immediately following the FTX (dates of collection Feb. 21–26, 2021). The majority of those testing positive were male (92.1%; n=151). The average age was 24, (range=7–43 years) with a majority in aged 20– 29 (71.3%; n=117). The majority were active duty soldiers (99.4%; n=163), with the remaining individual being a young (under 18 years old) family member of an active duty soldier. Battalion A accounted for 144 of the individuals testing positive (87.8%). Among the 154 individuals whose reasons for testing were specified, a majority experienced no symptoms (68.8%; n=106) while a minority did experience symptoms (n=48; 31.2%). No cases reported symptoms as being severe (data not shown). For an additional 10 individuals, no data were available as to whether they experienced symptoms (unspecified) (Table). The most common reason for testing was being identified as a close contact to a positive case only (62.2%; n=102).
During the peak outbreak period, 67.8% (97/143) of COVID-19 cases were asymptomatic close contacts who were tested primarily as the result of contact tracing efforts stemming from the index case (Table). Conversely, none of the cases during the pre-outbreak period and one-third (5/15) of the cases in the late-outbreak period were tested due to close contact. Furthermore, just one-quarter (36/143) of peak outbreak cases reported symptoms while two-thirds (4/6) of pre-outbreak cases and a little more than half (8/15) of late outbreak cases reported symptoms. Of note, at the time of this outbreak, COVID-19 vaccine was not widely available. Only 2 medics from the medical detachment were fully vaccinated. Neither of the vaccinated medics who were tested during the outbreak period contracted COVID-19 whereas 4 of the 5 unvaccinated medics tested positive for SARS-CoV-2.
Editorial Comment
This report describes a COVID-19 outbreak tied to a single military training event that affected almost a quarter (23.8%) of soldiers in an infantry battalion. The current findings demonstrate that highly contagious variants could be of particular concern in military congregate living settings, especially those with shared sleeping spaces. Disease severity during the outbreak was generally mild in an otherwise healthy population; however, the results underscore the negative impact (i.e., 24% of a battalion isolated or quarantined) that a COVID-19 outbreak, especially of a highly contagious variant, can have on readiness. Intensive contact tracing, testing, and command-implemented isolation and quarantine contributed to quick extinction of the outbreak. These control efforts resulted from an investigation of the outbreak that featured robust two-way communication between JBLM Public Health and the medical and command assets of the affected units.
In addition, the experience of the 2 vaccinated medics supports the effectiveness of vaccinations in combating COVID-19 transmission.
Military leaders are tasked with optimizing and maintaining combat readiness of their soldiers and the unit. The COVID-19 pandemic presents a unique challenge to leaders in balancing combat readiness against mitigation of SARS-CoV-2 transmission. Although this battalion's leadership took additional steps to ensure COVID-19 mitigation measures were incorporated into every aspect of the field training exercise, this outbreak was not prevented.
Three key issues appear to have contributed to this outbreak. First, the unit did not include pre-deployment COVID-19 screening as part of operational plans. Symptom-based or temperature-based screening might have mitigated viral transmission risk by identifying soldiers displaying symptoms of COVID-19 who needed to be tested and isolated prior to deployment. Furthermore, lab-based screening might have identified asymptomatic spreaders and potentially prevented this outbreak. As a result of this outbreak, the leadership of the training base has implemented a screening protocol for members of units undergoing training activities.
However, it should be noted that the apparent index case did not develop symptoms until the 13th day of the exercise, so pre-exercise screening might not have been helpful in detecting his infection.
Second, the unit's contingency plan for extreme weather conditions did not incorporate adequate COVID-19 mitigation measures in indoor settings. Overcrowded indoor sleeping arrangements coupled with poor ventilation permitted conditions for widespread transmission of a highly contagious variant of COVID-19. This was potentially exacerbated by transport back to JBLM on buses where large numbers of soldiers in a shared air space could also promote disease transmission. Given the exigency of protecting the soldiers from severe weather conditions, the local public health authority was not consulted about these decisions made prior to the recognition of the first COVID case in the unit.
Third, despite the index case presenting to the platoon aid station with report of chills and a fever on Feb. 16, 2021, 4 days before laboratory-confirmed diagnosis of SARS-CoV-2 infection, this soldier was not evaluated for COVID-19 or placed in isolation. Instead, the soldier was returned to duty. This misstep could have been averted through the use of an effective screening protocol that triggered isolation and testing for anyone presenting with symptoms consistent with COVID-19. Early removal and testing of the index case might have significantly reduced the number of positive cases in this outbreak.
This study has some limitations that should be considered in light of the findings. The lack of access to COVID-19 testing at YTC may have led to delayed diagnoses in some cases. In addition, the absence of a licensed independent medical provider at the training event may have also led to delayed diagnosis. The scope of practice for medics assigned to this exercise included provision of OTC medications for sick-call and ordering quarantine/isolation for possible communicable disease, although no such determination (isolation) was made for the index case.
This study describes the characteristics of a Beta variant outbreak which may not be fully applicable to other more current or emerging SARS-CoV-2 variants. This study also describes the characteristics of an outbreak in a predominantly unvaccinated population which is no longer applicable to the current predominantly vaccinated military force.
The findings of this study can inform mitigation efforts in military units in a deployed or field training environment and are particularly applicable in the setting of the Delta variant as the predominant cause of COVID-19. Like Beta, Delta is highly contagious, suggesting the need for continued vigilance among medical personnel and leaders at all levels during deployment and training events. Similarly, the planning considerations that might have mitigated or prevented the outbreak described in this report could be valuable for medical and command elements preparing for training or deployment events.
Author Affiliations: Madigan Army Medical Center, Department of Public Health, JBLM, WA (LTC Mease, MAJ Yun, CPT Egbert, LTC Yassin, COL Faestel, CPT Moyer, COL Terrio); Department of Chemistry and Life Science, United States Military Academy, West Point, NY (MAJ Bateman).
Acknowledgements: The authors thank MAJ Jeremy McGuffey for his assistance in collecting details of the field training exercise which made this work possible. The authors also thank LTC Kurt Jerke for his laboratory expertise and input.
Funding: All work described herein was performed as part of paid regular duties as part of employment by the U.S. Government.
Conflicts of Interest: None.
Disclaimer: The views expressed herein are those of the authors and do not necessarily represent the views of the U.S. Army, Department of Defense, or U.S. Government.
References
- Tracking SARS-CoV-2 variants. Accessed Jan. 28, 2022. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- Chappell B. South Carolina Reports 1st Known U.S. Cases Of Variant From South Africa. NPR. Published Jan. 28, 2021. Accessed Sept. 17, 2021. https://www.npr.org/sections/coronavirus-live-updates/2021/01/28/961609976/south-carolina-reports-1st-known-u-s-cases-of-variant-from-south-africa
- CDC. COVID Data Tracker. Centers for Disease Control and Prevention. Published March 28, 2020. Accessed Sept. 17, 2021. https://covid.cdc.gov/covid-data-tracker
- WA DOH. SARS-CoV-2 Sequencing and Variants in Washington State. Accessed April 15, 2021. https://www.doh.wa.gov/Portals/1/Documents/1600/coronavirus/data-tables/420-316-SequencingAndVariantsReport.pdf
- Pearson CAB, Russell TW, Davis NG, et al. Estimates of severity and transmissibility of novel SARS-CoV-2 variant 501Y.V2 in South Africa. CMMID Repository. Published Jan. 11, 2021. Accessed Sept. 17, 2021. https://cmmid.github.io/topics/covid19/sa-novel-variant.html
- CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. Published Feb. 11, 2020. Accessed Sept. 17, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html
- Madhi SA, Baillie V, Cutland CL, et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 Vaccine against the BETA Variant. New Engl J Med. 2021;384(20):1885–1898.
- Mahase E. Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant. BMJ. 2021;372:n296.
- What you need to know about the 501Y.V2 (BETA) South African Variant of SARS-CoV-2. Ask a Scientist. Published Jan. 19, 2021. Accessed Sept. 17, 2021. https://www.thermofisher.com/blog/ask-a-scientist/what-you-need-to-know-about-the-501y-v2-b-1-351-south-african-variant-of-sars-cov-2/
- CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. Published Feb. 11, 2020. Accessed Sept. 17, 2021. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/scientific-brief-emerging-variants.html
- HQ, Department of the Army, Facility Sanitation Controls and Inspections. March 1, 2019. TB MED 531: 44-45. Accessed Sept. 17, 2021. https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN16903_tbmed531_FINAL.pdf