Colorectal cancer, which is more predominant among men than women, has been shown to be associated with environmental and occupational risk factors experienced by military members. The Defense Medical Surveillance System was used to determine the crude and age-adjusted incidence rates of colorectal cancer among active component service members from all military services from January 1, 2010 to December 31, 2022. Results from this analysis show higher crude incidence rates of colorectal cancer among those who are older and male. The overall age-adjusted incidence rate throughout the surveillance period ranged from 3.56 (95% CI: 2.54-4.58) to 7.92 (95% CI: 5.98-9.86) cases per 100,000 person-years. Age-adjusted colorectal cancer rates were similar for males and females (4.46 and 4.33 cases per 100,000 person-years, respectively) and rates were relatively similar by service as well as race and ethnicity. This finding could be attributed to the small number of cases in this study due to better screening practices in the Military Health System.
What are the new findings?
Although non-Hispanic Black service members have historically had the highest incidence of colorectal cancer within the U.S. military, this study observed similar rates of colorectal cancer for all races and ethnicities after adjusting for age.
What is the impact on readiness and force health protection?
Incident rates of colorectal cancer within the U.S. military increase monotonically with age, with service members over the age of 45 with the highest incidence, re-enforcing the need to promote wellness screening among military populations. The importance of the DHA guideline changes that decreased colorectal screenings to age 45 years is significant.
Background
Colorectal cancer is the third-most common cancer in incidence and mortality in the U.S.1 Even though incidence of other digestive cancers such as liver and pancreatic cancers increased during the past 20 years,2 colorectal cancer incidence in the U.S. decreased during the same period among adults aged 50 years and older.3 This decrease in colorectal cancer is partly due to increased screening, leading to early detection and treatment of pre-cancerous lesions.4
Colorectal cancer can be caused by exposure to risk factors such as tobacco use, alcohol use, diet, body composition, and physical inactivity.5-9 There is also evidence showing an association between colorectal cancer and environmental and occupational risk factors.10-13 Active component service members (ACSM) tend to be generally healthier than the U.S. general population, but they also tend to have a higher prevalence of smoking and alcohol use, and are more likely to be exposed to occupational risk factors including radiation, particulate matter, and solvents linked to colorectal cancer.11-13
Overall, rates of colorectal cancer in U.S. military service members are lower compared to age-adjusted rates within the general U.S. population.14,15 In a study assessing incidence of numerous cancers from 2005 to 2014, the rate of colorectal cancer among ACSM was 4.5 cases per 100,000 person-years (p-yrs), with higher rates among men and African Americans.16 Another study of colorectal cancer specifically identified 1,108 incident cases of colorectal cancer among ACSM from 1997 to 2016, with a higher incident rate among men (4.4 per 100,000 p-yrs) as well as non-Hispanic Black service members (5.3 per 100,000 p-yrs).17 This study aims to build on prior analyses of incident colorectal cases among ACSM17 and describe the incidence rate of colorectal cancer among active component U.S. military service members between 2010 and 2022.
Methods
The results presented in this study include ACSM from all military services from January 1, 2010 through December 31, 2022. Data were obtained from the Defense Medical Surveillance System. Demographic data on age, military service, race and ethnicity, rank, and occupation at the time of colorectal cancer diagnosis were included. Ambulatory and inpatient administrative health records from both direct and Click to closePurchased CareThe TRICARE Health Program is often referred to as purchased care. It is the services we “purchase” through the managed care support contracts.purchased care were used to determine colorectal cancer diagnoses.
Case definition
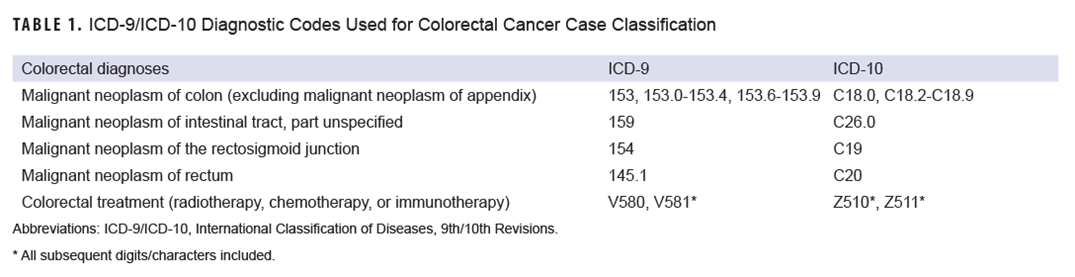
International Classification of Diseases, 9th/10th revision diagnostic codes, along with V-codes and Z-codes indicating a qualifying treatment (radiotherapy, chemotherapy, or immunotherapy), were used to define incident cases of colon and rectum cancer (Table 1).18 Cases of appendiceal malignancies were excluded, as they are histologically different from colorectal cancer.18 An incident case of colorectal cancer was defined as either one hospitalization with a qualifying ICD-9 or ICD-10 diagnosis code in the first diagnostic position, or in the second diagnostic position if a V/Z-code indicating radiotherapy, chemotherapy, or immunotherapy treatment was in the first diagnostic position; or three or more ambulatory encounters within a 90-day period with a qualifying ICD-9/10 diagnostic code in the first or second diagnostic position.18
The date of the first case-defining hospitalization or ambulatory medical encounter was used as the incident date. Service members were counted once per lifetime. Person-time contributions for each service member were determined from January 1, 2010 to December 31, 2022. Service members and their person-time contributions were removed from the study population if a case-defining encounter was recorded prior to the start of the surveillance period on January 1, 2010. Person-time was censored when a service member left the active component or military service, and at the time of the incident diagnosis for a colorectal cancer case, whichever occurred first.
Statistical analysis
Crude and age-adjusted incident rates were calculated as incident colorectal cancer diagnoses per 100,000 p-yrs with 95% confidence intervals. The standard population used for the age-adjustment was the Military Health System ACSM population in DMSS from 2010 to 2022, and age groups were utilized for adjusting colorectal incident rates. This age adjustment gave more weight to the younger age groups that constitute a majority of the ACSM population, leading to more stable incident rates. Incident rate ratios and 95% CI were calculated to compare colorectal cancer rates by all demographic variables included in the study. All analyses were conducted using SAS (version 9.4) with a significance level set at p<0.05.
Results
During the 13-year surveillance period 741 incident cases of colorectal cancer among ACSM were recorded, corresponding to an overall crude incident rate of 4.44 (95% CI: 4.12-4.76) cases per 100,000 p-yrs (Table 2). The average age among colorectal cancer cases during the surveillance period was 39.9 years (STD=7.9, range 20-59). The distributions of incident colorectal cancer cases by select demographic characteristics are detailed in Table 2.
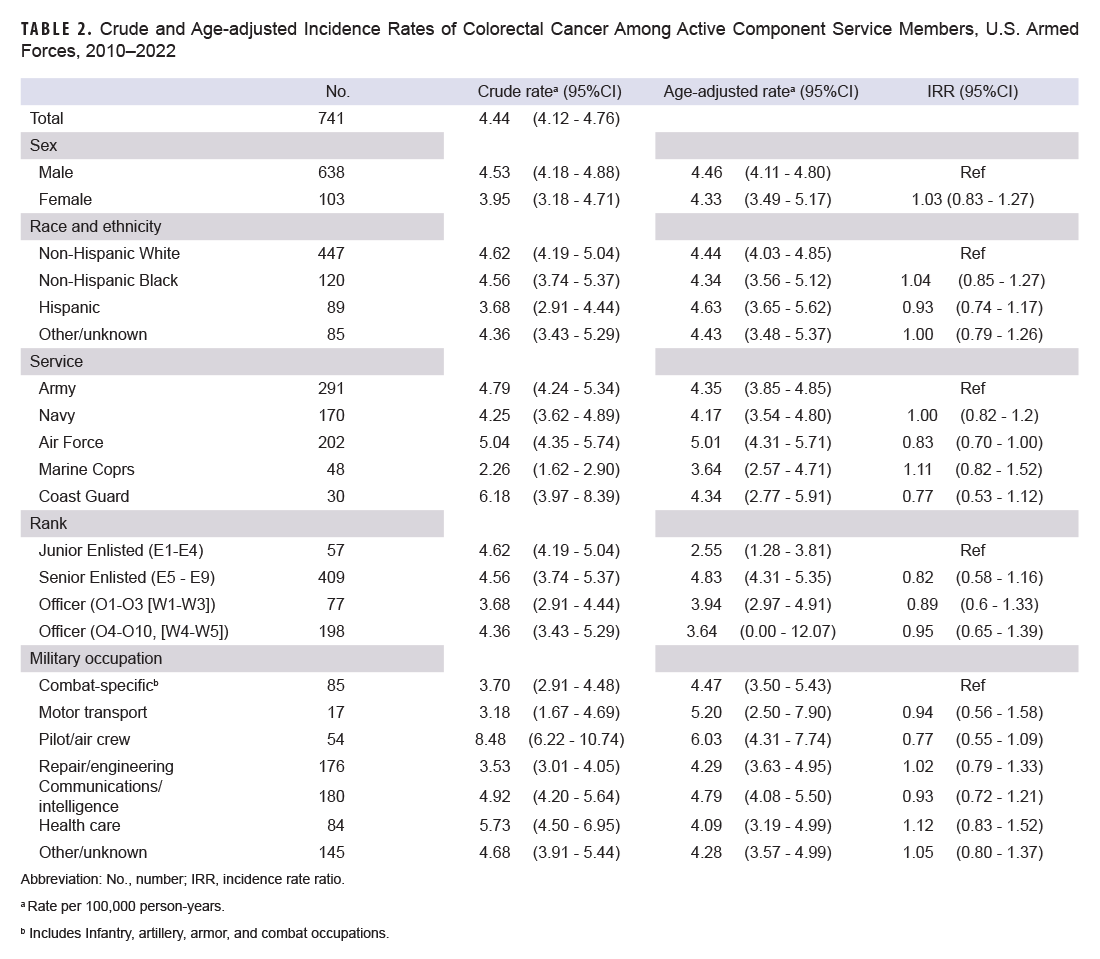
Crude incidence rates were higher among men and increased with age, ranging from 0.41 (95% CI: 0.24-0.57) per 100,000 p-yrs among those ages 20-24 to 54.51 (95% CI: 42.64-66.38) per 100,000 p-yrs among those older than 50-54 years (Table 2). Only a few cases were recorded in the 55 and older age group (n=14), with some years—2013, 2015, 2019, 2021, 2022—reporting zero cases in the oldest age group (data not shown).
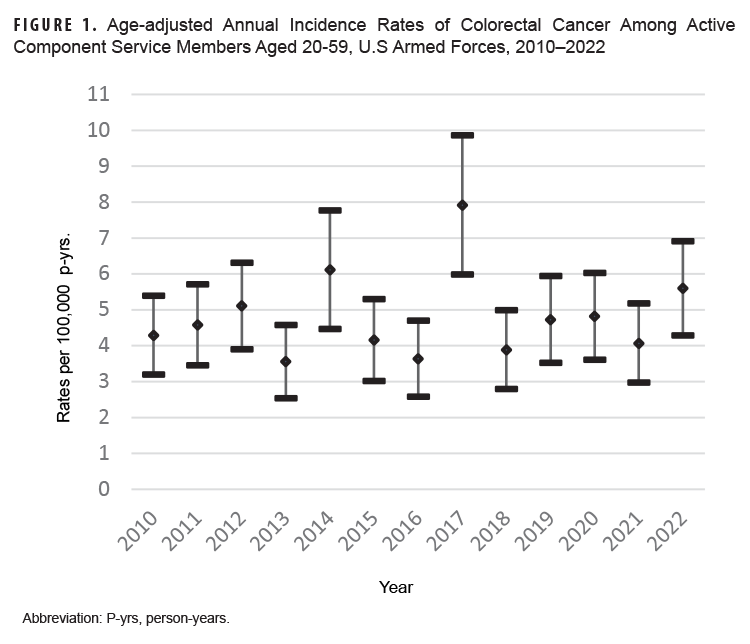
The overall age-adjusted incidence rate throughout the surveillance period ranged from 3.56 (95% CI: 2.54-4.58) to 7.92 (95% CI: 5.98-9.86) cases per 100,000 p-yrs (Figure 1). The age-adjusted incidence rate peaked in 2017, at 7.92 (95% CI: 5.98-9.86) cases per 100,000 p-yrs, and then fluctuated for the rest of the surveillance period (Figure 1).
Age-adjusted colorectal rates were similar for men and women (4.46 [95% CI: 4.11-4.80] and 4.33 [95% CI: 3.49-5.17] cases per 100,000 p-yrs, respectively), and rates were relatively similar by service (Table 2).
Age-adjusted rates were also similar for all races and ethnicities, ranging from 4.34 (95% CI: 3.56-5.12) cases per 100,000 p-yrs among non-Hispanic Blacks to 4.63 (95% CI: 3.65-5.62) cases per 100,000 p-yrs among Hispanics (Table 2). The incident rate ratio was also relatively similar for all races and ethnicities, with no statistical significance when compared to non-Hispanic Whites (Table 2).
Service members in the pilot/air crew occupation category had the highest age-adjusted colorectal incident rate (6.03 [95% CI: 4.31-7.74]), followed by those in motor transportation (5.20 [95% CI: 2.50-7.90]) (Table 2). There was no significant difference, however, in the incident rate ratio for all occupation groups when compared to the reference group (infantry/artillery/armor/combat) (Table 2).
Discussion
This analysis shows a higher crude incidence rate of colorectal cancer among those 50 to 54 years of age; a previous study of the active component military population, from 1997 to 2016, found similar results.17 Age-adjusted colorectal cancer incident rates did not show any temporal trends during the study period, except for an increase in 2017. The prior study of colorectal cancer among ACSM from 1997 to 2016 also observed no temporal trends after adjusting for age.17 The lack of temporal trends in the military population diverges from general U.S. population data, which from 2011 to 2019 have shown a 1% annual decrease.19 This difference between the two populations could be due to the limited number of cases among ACSM, in turn leading to few cases among the younger (20-29 years) and older (55+ years) age groups.
The high incidence of colorectal cancer among service members in the pilot/aircrew occupation correlates with prior surveillance reports.17 While this occupation accounts for the highest rate of colorectal cancer, a recent study of military pilots showed evidence that aircrew colorectal cancers were statistically lower in the military population when compared to the general U.S. population, by 44%.20,21 Lower rates among ACSM may be attributed to universal health care and improved access to screenings for early pre-cancerous detection and treatment.
Older, White males have historically demonstrated greater use of colorectal cancer screenings within the MHS.22 This study did not observe, after adjusting for age, any significant colorectal cancer rate differences between races and ethnicities (Table 2) that could indicate racial differences in health care access and screening. Recent Defense Health Agency guideline changes that lowered the recommended age for colorectal screenings to age 45, combined with promotion of non-invasive colorectal cancer screenings and universal health care for all ACSM, may be contributing factors to the uniform incident rate among races and ethnicities.22,23 Continued surveillance of colorectal cancer among ACSM is necessary for understanding the true burden of colorectal cancer within the MHS.
One of this study's primary limitations is that it did not use the DOD’s cancer registry system, Oncolog, formerly known as the ACTUR. Oncolog includes cancer data reported by military hospitals and clinics for all DOD beneficiaries. Because this study relies solely on medical encounter data and does not incorporate Oncolog case reports, it may not include all colorectal cancer cases. Further studies should include both Oncolog and medical encounter data. Efforts are currently underway to determine true estimates of cancer diagnoses and treatment outside the MHS through the incorporation of data shared from state cancer registries.24
This study did not adjust for modifiable risk factors shown to increase risk of colorectal cancer such as obesity, physical inactivity, smoking, alcohol consumption, or environmental exposures.5-10 The active component military population tends to be engaged in more physical activity, is required to pass routine physical fitness examinations, and must maintain a healthy body weight, and thereby is less likely to be overweight or obese compared to the general U.S. population.21 These protective factors can be accredited to overall lower colorectal incidence rates within the U.S. military. Exposure to environmental toxins attributed to increased risk of colorectal cancer may be greater in this group, however, especially during deployment. Including deployment location and length of deployment in further analyses is important.
Author Affiliations
Defense Health Agency, Armed Forces Health Surveillance Division, Silver Spring, MD: Dr. Mabila, Ms. McQuistan, Ms. Murray.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the official policy of the Department of Defense nor the U.S. Government.
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21654
- Gordon-Dseagu VL, Devesa SS, Goggins M, Stolzenberg-Solomon R. Pancreatic cancer incidence trends: evidence from the Surveillance, Epidemiology and End Results (SEER) population-based data. Int J Epidemiol. 2018;47(2):427-439. doi:10.1093/ije/dyx232
- Siegel RL, Torre LA, Soerjomataram I, et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut. 2019;68(12):2179-2185. doi:10.1136/gutjnl-2019-319511
- Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683-691. doi:10.1136/gutjnl-2015-310912
- National Center for Chronic Disease Prevention Health Promotion Office on Smoking Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention (U.S.); 2014.
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2014:1-14. doi:10.1038/bjc.2014.579
- World Cancer Research Fund International, American Institute for Cancer Research. Meat, Fish and Dairy Products and the Risk of Cancer: Continuous Update Project Expert Report. 2018.
- World Cancer Research Fund International, American Institute for Cancer Research. Wholegrains, Vegetables and Fruit and the Risk of Cancer: Continuous Update Project Expert Report. 2018.
- World Cancer Research Fund International, American Institute for Cancer Research. Other Dietary Exposures and the Risk of Cancer: Continuous Update Project Expert Report. 2018.
- Matich EK, Laryea JA, Seely KA, Stahr S, Su LJ, Hsu PC. Association between pesticide exposure and colorectal cancer risk and incidence: a systematic review. Ecotoxicol Environ Saf. 2021;219:112327. doi:10.1016/j.ecoenv.2021.112327
- Weese CB, Abraham JH. Potential health implications associated with particulate matter exposure in deployed settings in southwest Asia. Inhal Toxicol. 2009;21(4):291-296. doi:1080/08958370802672891
- Aurell J, Gullett BK, Yamamoto D. Emissions from open burning of simulated military waste from forward operating bases. Environ Sci Technol. 2012;46(20):11004-11012. doi:10.1021/es303131k
- Lowers HA, Todorov R, Strand MJ, et al. Lung biopsies from symptomatic military deployers have variable mineral particle types and higher abundances of silicon, aluminum, cadmium and vanadium compared to controls. Am J Respir Crit Care Med. 2015;191:A2575.
- Zhu K, Devesa SS, Wu H, et al. Cancer incidence in the U.S. military population: comparison with rates from the SEER program. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1740-1745.
- Bytnar JA, Shriver CD, Zhu K. Incidence rates of digestive cancers among U.S. military servicemen: comparison with the rates in the general U.S. population. PLoS One. 2021;16(9):e0257087. doi:10.1371/journal.pone.0257087
- Lee T, Williams VF, Clark LL. Incident diagnoses of cancers in the active component and cancer-related deaths in the active and reserve components, U.S. Armed Forces, 2005-2014. MSMR. 2016;23(7):23-31.
- Stahlman S, Oetting A. Age-period-cohort analysis of colorectal cancer, service members aged 20-59 years, active component, U.S. Armed Forces, 1997-2016. MSMR. 2017;24(7):12-19.
- Armed Forces Health Surveillance Division. Surveillance Case Definition. Colorectal Cancer. Nov. 2022. www.health.mil/Reference-Center/Publications/2022/11/01/Colorectal-Cancer
- Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023;73(3):233-254.
- Department of Defense. Study on Incidence of Cancer Diagnoses and Mortality Among Military Aviators and Aviation Support Personnel. 2023. https://www.health.mil/Reference-Center/Reports/2023/02/09/Study-on-the-Incidence-of-Cancer-Diagnosis-and-Mortality-among-Military-Aviators-and-Aviation-Support-Personnel
- Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109(8):djw322. doi:10.1093/jnci/djw322
- Debarros M, Steele SR. Colorectal cancer screening in an equal access healthcare system. J Cancer. 2013;4(3):270-280. doi:10.7150/jca.5833
- Hammer, R. Colorectal Cancer Screening Age Decreases to 45. Accessed Apr. 27, 2023. https://health.mil/News/Articles/2022/11/22/Colorectal-Cancer
- Stahlman S, Clerkin C, Kohler B, Howe W Jr, Cronin K, Wells N. Brief report: Phase I results using the virtual pooled registry cancer linkage system for military cancer surveillance. MSMR. 2022;29(7):26-27.