Abstract
The current report used an ocular and vision disease classification system and several health care burden measures to quantify the impacts of various ocular and vision-related illnesses and injuries among active component service members of the U.S. Armed Forces during 2018. More service members received care for refractive error and related disorders than any other ocular and vision-related major category; this category accounted for slightly more than one-half (51.1%) of all ocular and vision-related medical encounters. Conjunctival disorders accounted for the next highest percentage of total medical encounters (13.3%) followed by corneal disorders (7.5%). The 3 specific ocular and vision-related conditions that accounted for the most medical encounters (i.e., myopia, astigmatism, and acute conjunctivitis) accounted for almost one-half (47.7%) of all ocular and vision-related medical encounters overall. In general, the conditions that accounted for the most medical encounters were predominantly refractive error and related disorders and conjunctival disorders. More active component service members received medical care for myopia than for any other specific condition. Optic nerve conditions and visual discomfort/disturbances accounted for more than one-quarter (30.1%) of all ocular and vision-related hospital bed days.
What Are the New Findings?
This is the first MSMR report specifically focused on the burden of ocular and vision conditions among active component U.S. service members. Refractive errors accounted for the majority of eye-related encounters among service members. Neuro-ophthalmic diagnoses (conditions of the optic nerve, visual tract, and cranial nerves responsible for eye movements) accounted for the most hospital bed days.
What Is the Impact on Readiness and Force Health Protection?
Eye health and optimal visual function are key to performance of military duties across the services. Effective prioritization of the magnitude and burden of ocular and visual conditions is essential to inform the targets for prevention, allocation of resources, training objectives, and research goals.
Background
Routinely collected health care utilization data are available for the U.S. Armed Forces and are regularly analyzed to inform prevention planning and resourcing.1 The Armed Forces Health Surveillance Branch produces annual reports of overall health care burden measures for ongoing evaluation.2 Accurate characterization of the frequency and impact of conditions affecting specific systems, such as the visual system, is essential. Degraded visual function can have a significant impact on both readiness and retention of service members. Financial costs of ocular injuries and visual dysfunction resulting from traumatic brain injury have been recently reported and are significant.3
Conditions of the eyes and visual system are responsible for considerable morbidity globally and have increased in incidence over time.4,5,6 Many of these conditions increase in frequency with advancing age.5 U.S. active component service members are a select subgroup of the population. As a result, the morbidity burden among service members may be significantly different from that in the general U.S. population. In addition, the U.S. military has rigorous standards for accession, including those for ocular conditions and visual acuity.7 The challenges to military operational performance due to eye and vision problems often do not have direct correlates in the civilian population.
Because of the unique nature of ocular and vision problems, these conditions usually require monitoring and treatment by dedicated eye care professionals. Population-level evaluation of these conditions is necessary to characterize their effects across the active component and to identify needed enterprise-wide priorities within a specialized system of care. Effective characterization of the magnitude and impact of these conditions will inform the targets for prevention, allocation of resources, training objectives, and research goals.
The current report used an ocular and vision disease classification system and several health care burden measures to quantify the impacts of various ocular and vision-related illnesses and injuries among active component service members of the U.S. Armed Forces during 2018. This approach will allow for interpretation of data in the context of conditions across the active component and identification of specific conditions for further assessment of the impacts on operational performance.
Methods
The surveillance period was 1 Jan. through 31 Dec. 2018. The surveillance population included all individuals who served in the active component of the U.S. Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. All data used in this analysis were derived from records routinely maintained in the Defense Medical Surveillance System (DMSS). These records document both ambulatory encounters and hospitalizations of active component service members of the U.S. Armed Forces in fixed military and civilian (if reimbursed through the Military Health System [MHS]) treatment facilities worldwide.
For this analysis, DMSS data for all inpatient and outpatient medical encounters of all active component service members during 2018 were summarized according to the primary (first-listed) diagnosis (if reported with an International Classification of Diseases, 10th Revision [ICD-10] code) for ocular and vision-related conditions. For summary purposes, ocular and vision-specific diagnoses (as defined by the ICD-10) were grouped into 128 subcategories and 24 main categories by clinical and public health subject matter experts at the Department of Defense/Veterans Affairs Vision Center of Excellence. The groupings were designed for maximal capture of conditions, allowing for expected variability in diagnostic coding.
The "morbidity burdens" attributable to various ocular and vision-related "conditions" were estimated based on the total number of medical encounters attributable to each condition (i.e., total hospitalizations and ambulatory visits for the condition with a limit of 1 encounter per individual per condition per day), numbers of service members affected by each condition (i.e., individuals with at least 1 medical encounter for the condition during the year), and total bed days during hospitalizations for each condition.
The new electronic health record for the MHS, MHS GENESIS, was implemented at several military treatment facilities during 2017. Medical data from sites that are using MHS GENESIS are not available in the DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounters for individuals seeking care at any of these facilities during 2018 were not included in this analysis.
Results
Morbidity burden, by category
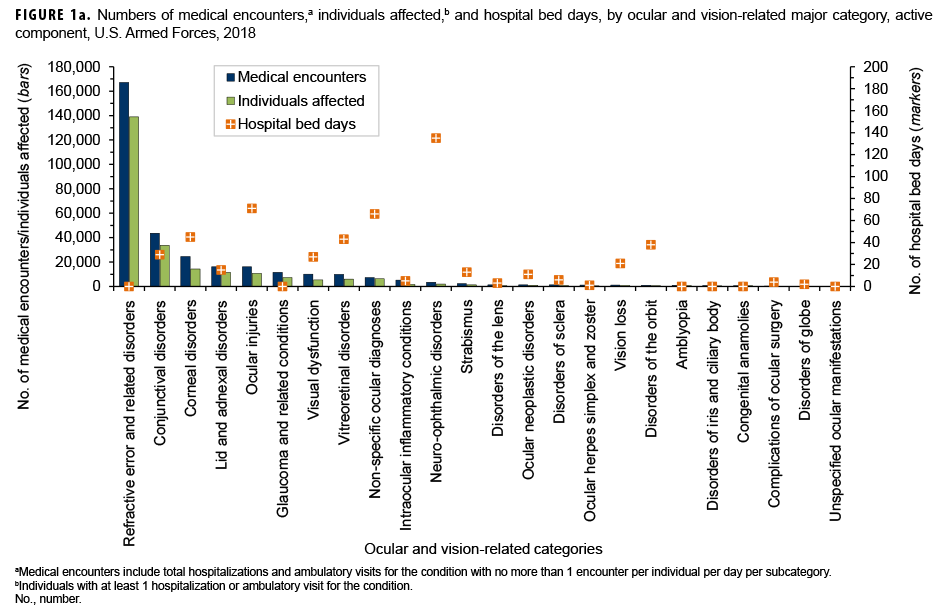
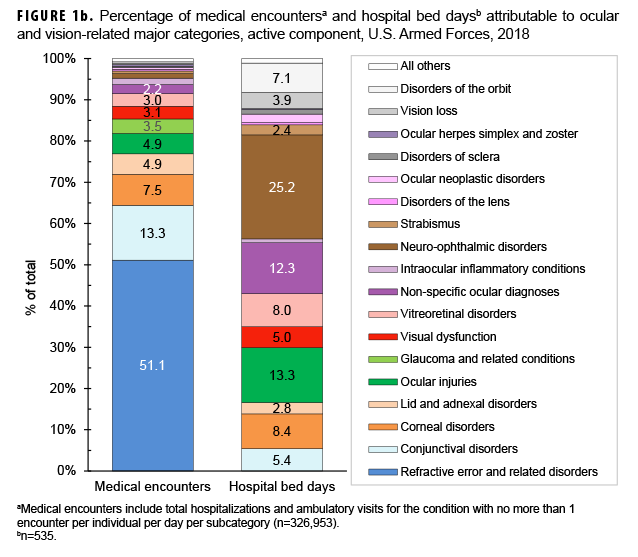
In 2018, more active component service members (n=138,961) received care for refractive error and related disorders than any other ocular and vision-related major category (Figure 1a); this category accounted for slightly more than one-half (51.1%) of all ocular and vision-related medical encounters (Figure 1b). Conjunctival disorders accounted for the next highest percentage of total medical encounters (13.3%) followed by corneal disorders (7.5%).
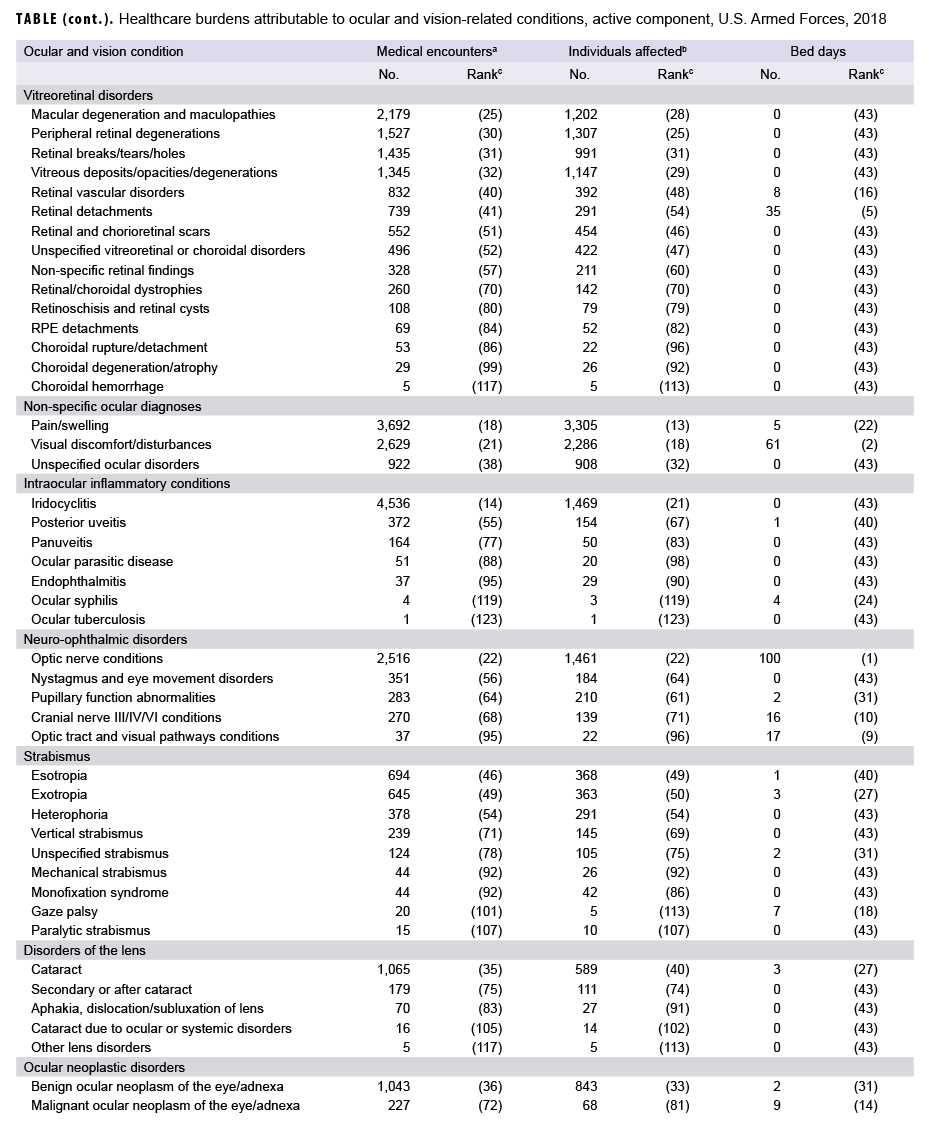
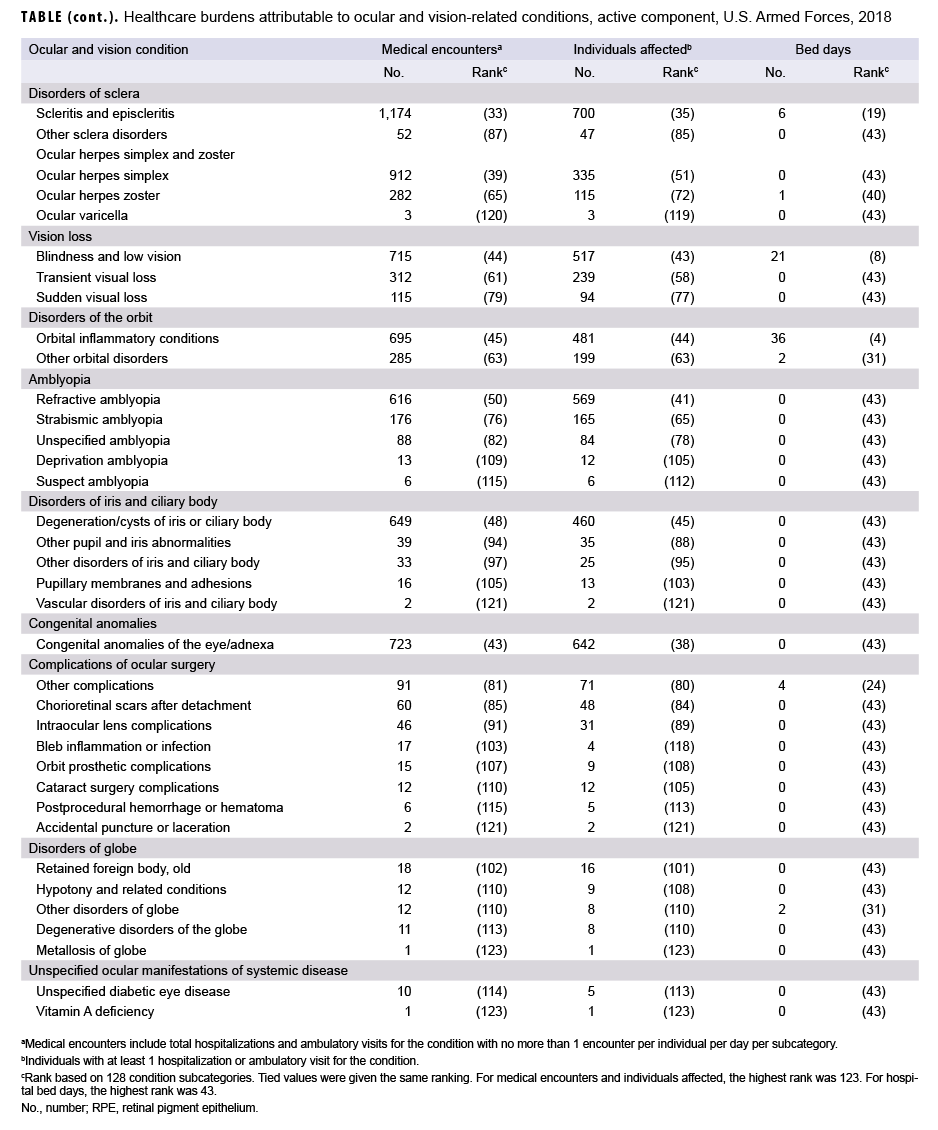
Ocular and vision-related conditions were associated with a total of 535 hospital bed days in 2018. Neuro-ophthalmic disorders accounted for slightly more than one-quarter (25.2%) of the total hospital bed days (Figure 1b). Together, neuro-ophthalmic disorders, ocular injuries, non-specific ocular diagnoses, corneal disorders, and vitreoretinal disorders accounted for more than two-thirds (67.3%) of all ocular and vision-related hospital bed days.
Medical encounters, by condition
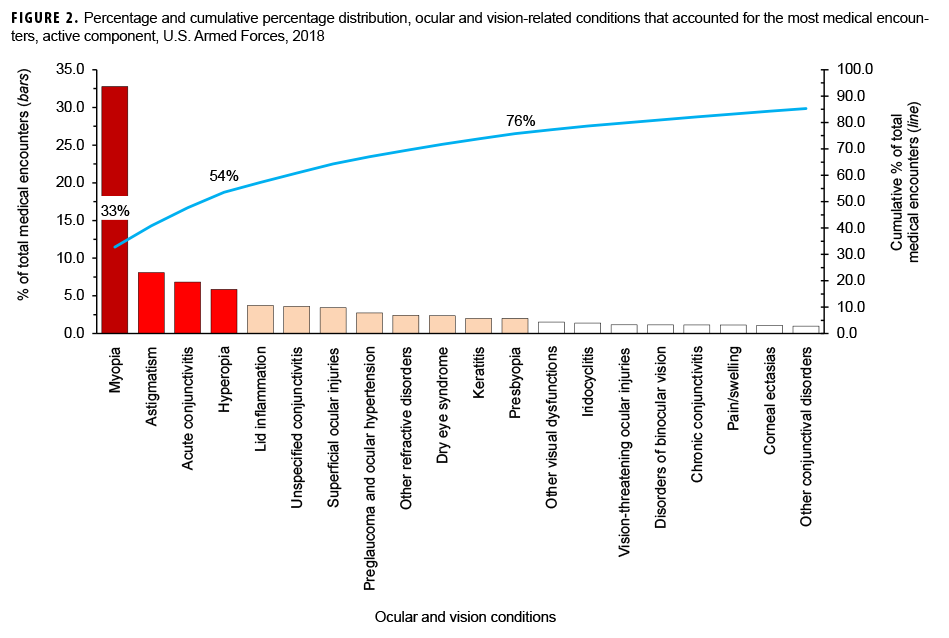
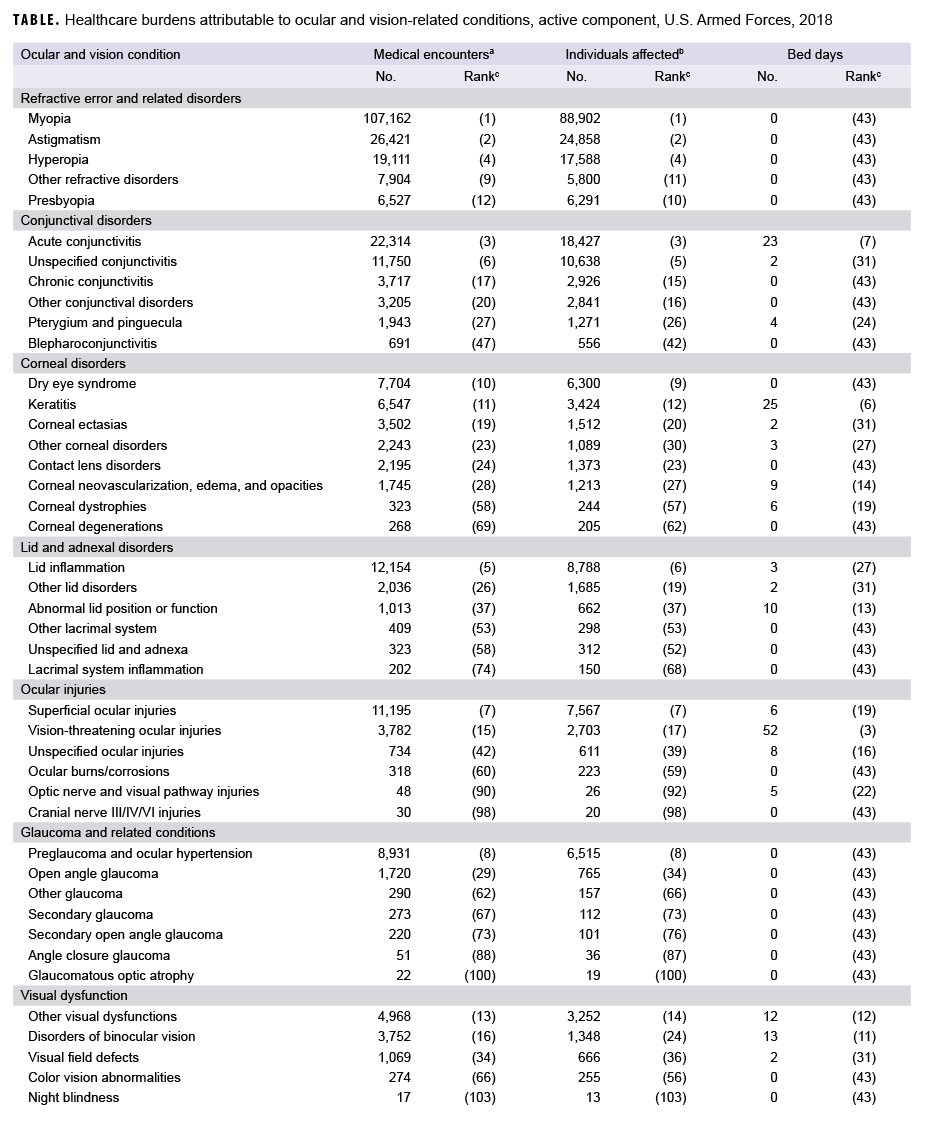
In 2018, the 3 ocular and vision-related conditions that accounted for the most medical encounters (i.e., myopia, astigmatism, and acute conjunctivitis) accounted for almost one-half (47.7%) of all ocular and vision-related medical encounters overall (Figure 2). Moreover, the top 8 conditions that accounted for the most medical encounters accounted for more than two-thirds (67.0%) of all medical encounters overall. In general, the conditions that accounted for the most medical encounters were predominantly refractive error and related disorders (e.g., myopia, astigmatism, hyperopia) and conjunctival disorders (e.g., acute conjunctivitis, unspecified conjunctivitis) (Table).
Individuals affected, by condition
In 2018, more active component service members received medical care for myopia than for any other specific condition (Table). Of the top 10 ocular and vision-related conditions that affected the most service members, 4 were refractive error and related disorders (myopia, astigmatism, hyperopia, and other refractive disorders); 2 were conjunctival disorders (acute conjunctivitis and unspecified conjunctivitis); 1 was a lid and adnexal disorder (lid inflammation); 1 was an ocular injury (superficial ocular injuries); 1 was a glaucoma and related condition (preglaucoma and ocular hypertension); and 1 was a corneal disorder (dry eye syndrome).
Hospital bed days, by condition
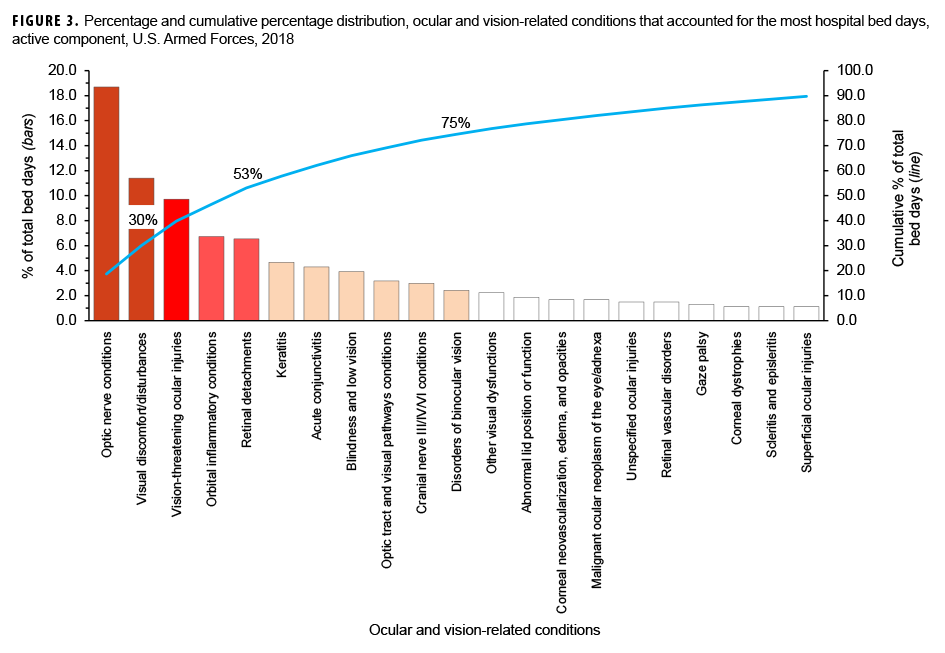
In 2018, optic nerve conditions and visual discomfort/disturbances accounted for more than one-quarter (30.1%) of all ocular and vision-related hospital bed days (Figure 3). Together, vision-threatening ocular injuries, orbital inflammatory conditions, and retinal detachments accounted for an additional 23.0% of the total hospital bed days.
Relationships between health care burden indicators
There was a strong positive correlation between the number of ocular and vision-related medical encounters attributable to various conditions and the number of individuals affected by the conditions (r=0.99) (data not shown). For example, the 6 leading causes of medical encounters were the 6 conditions that affected the most individuals (Table). In contrast, there were very weak linear relationships between the hospital bed days attributable to ocular and vision-related conditions and either the numbers of individuals affected by (r=0.02) or medical encounters attributable to (r=0.05) the same conditions (data not shown).
Editorial Comment
This is the first MSMR report on the burden of ocular and vision conditions among U.S. active component service members. Three of the 24 major categories (refractive error and related disorders, conjunctival disorders, and corneal disorders) accounted for 72.0% of medical encounters during 2018. However, these same categories accounted for less than one-sixth (13.8%) of the total hospital bed days in 2018.
Refractive error and related disorders accounted for the most medical encounters and individuals affected; this category of conditions has specific readiness standards and, as such, the data reported here can provide insight into the burden of maintaining these requirements. Myopia, astigmatism, and hyperopia accounted for the vast majority (91.4%) of refractive error–related medical encounters. The significance of these conditions in relation to military readiness and performance is discussed in greater detail in a later report in this MSMR issue.8
Several of the categories examined in this analysis could have significant impacts on readiness and/or retention because of their potential for prolonged or permanent effects on visual performance. Ocular injuries accounted for 4.9% of total medical encounters and 13.3% of total hospital bed days. Out of the total ocular injury–related medical encounters reported in 2018, slightly more than one-quarter (25.9%) were for non-superficial injuries (i.e., vision-threatening injuries, burns/corrosions, visual pathway injuries, and cranial nerve III/IV/VI injuries); non-superficial ocular injuries accounted for more than three-quarters (80.3%) of ocular injury–related hospital bed days.
Vitreoretinal conditions, which affect the posterior structures of the eye and often require subspecialist assistance in diagnosis and management, accounted for 2.6% of total medical encounters and 8.0% of total hospital bed days. Neuro-ophthalmic diagnoses (conditions of the optic nerve, visual tract, and cranial nerves responsible for eye movements) accounted for only 1.1% of all medical encounters but approximately one-quarter (25.1%) of total hospital bed days. Of note, complications of ocular surgeries accounted for less than 0.1% of encounters.
This report also allows for framing the burden of eye and vision conditions in the context of overall burden of disease across the active component. For example, in comparison to the other 141 specific conditions examined in the MSMR's annual analysis of the health care burden of diseases and injuries, disorders of refraction and accommodation ranked 18th in terms of the numbers of outpatient encounters and 7th in the numbers of service members affected. Refractive error and related disorders affected more individuals than either arm and shoulder injuries or leg injuries (although with considerably fewer attributable encounters).2 Relationships between health care burden indicators were similar to those observed with overall disease burden among active component service members.2 When comparing numbers of medical encounters to numbers of individuals affected, there was a strong positive correlation. When comparing hospital bed days attributable to conditions to numbers of individuals affected or to medical encounters attributable to the same conditions, there were very weak linear relationships. Many ocular and vision-related categories had zero bed days attributed to that category. In general, these correlations are consistent with the trend of eye care, especially ocular surgery, being provided in an ambulatory care setting.9
This report is subject to several limitations. As noted above, the change in electronic health record systems to MHS GENESIS removed data from multiple treatment facilities for this analysis, leading to underreporting of total numbers. In 2018, 6,396 active component service members received care for non-specific ocular diagnoses, and this category accounted for 12.3% of total hospital bed days in 2018. It is important to recall that this summary of the burden of ocular and vision conditions was limited to encounters in which such diagnoses were in the first diagnostic position of records. This method would exclude a relatively large number of ocular conditions related to encounters for other conditions listed in the first diagnostic position, such as trauma and respiratory tract infections. In addition, further exploration is needed to ascertain the final diagnoses determined for those affected by non-specific ocular diagnoses.
In summary, this initial report on the relative burden of ocular and vision conditions is critical to ongoing efforts to quantify the effects of ocular and vision conditions on the readiness of service members. The findings of the current analysis provide targets for further surveillance reports as well as conditions requiring further exploration using readiness and retention data. As with overall burden of illness and injury reports, ocular and vision conditions identified will inform key prevention, mitigation, and rehabilitation strategies.
Author affiliations: Department of Defense/Veterans Affairs Vision Center of Excellence, Defense Health Agency Research and Development Directorate (COL Reynolds); Defense Health Agency, Armed Forces Health Surveillance Branch (Ms. Williams, Dr. Taubman, Dr. Stahlman)
Disclaimer: The contents, views, or opinions expressed in this publication are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency, Department of Defense, or the U.S. Government.
References
- Brundage JF, Johnson KE, Lange JL, Rubertone MV. Comparing the population health impacts of medical conditions using routinely collected health care utilization data: Nature and sources of variability. Mil Med. 2006;171(10):937–942.
- Armed Forces Health Surveillance Branch. Absolute and relative morbidity burdens attributable to various illnesses and injuries, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):2–10.
- Frick KD, Singman EL. Cost of military eye injury and vision impairment related to traumatic brain injury: 2001–2017. Mil Med. 2019;184(5–6):338–343.
- Ono K, Hiratsuka Y, Murakami A. Global inequality in eye health: country-level analysis from the Global Burden of Disease Study. Am J Public Health. 2010;100(9):1784–1788.
- Finger RP, Fimmers R, Holz FG, Scholl HP. Incidence of blindness and severe visual impairment in Germany: projections for 2030. Invest Ophthalmol Vis Sci. 2011;52(7):4381–4389.
- Foran S, Wanj JJ, Rochtchina E, Mitchell P. Projected number of Australians with visual impairment in 2000 and 2030. Clin Exp Ophthalmol. 2000;28(3):143–145.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6130.03. Medical Standards for Appointment, Enlistment, or Induction in the Military Services. 6 May 2018.
- Reynolds ME, Taubman S, Stahlman S. Incidence and prevalence of selected refractive errors, active component, U.S. Armed Forces, 2001–2018. MSMR. 2019;26(9):26–30.
- Stagg BC, Talwar N, Mattox C, Lee PP, Stein JD. Trends in use of ambulatory surgery centers for cataract surgery in the United States, 2001–2014. JAMA Ophthalmol. 2018;136(1):53–60.