Background
Heat injury surveillance in the Department of Defense (DOD) includes the more severe conditions, heat exhaustion and heat stroke.1 Hospitalization occurs more frequently among service members experiencing heat stroke; however, both conditions can result in hospitalization and may require follow-up medical care. Between 2014 and 2018, annual rates of heat illness have increased among U.S. active component members.2 This report describes the total direct medical cost to the Army associated with heat exhaustion and heat stroke from 2016 through 2018.
Methods
The Weather-Related Injury Repository (WRIR) contains clinical data and medical event reports for heat and cold weather injuries in Army soldiers.3 The WRIR health encounter and admission data used in this analysis were derived from DOD military medical treatment facility medical records and paid TRICARE claims for beneficiaries at civilian facilities. Heat illness was identified using International Classification of Diseases, 10th Revision (ICD-10) codes for heat stroke (T67.0*) and heat exhaustion (T67.3*, T67.4*, T67.5*) in the primary or secondary diagnostic code positions.1For the purposes of this study, heat illness hospital admissions and outpatient encounters from 1 Jan. 2016 through 31 Dec. 2018 were extracted from the WRIR for Army active component and active and inactive National Guard and Reserve soldiers. Demographic characteristics were assigned according to the first encounter or admission during the analysis timeframe for each soldier.
Direct medical costs from the medical record and claims files were used to represent the cost of care paid for by the Military Health System (MHS). Variables for these costs have been included in the WRIR for each encounter since its implementation. For inpatient admissions to facilities owned and operated by the military, the direct cost of the care is captured in a variable identified as "full cost," which includes the cost of clinician salary, ancillary laboratory and radiology, ancillary salary, and intensive and surgical care units. For outpatient visits associated with these facilities, the direct cost of care captured in the same full cost variable includes clinician salary, professional salary, laboratory, radiology, pharmacy, ancillary, support, and other costs. For contracted care provided in civilian or network facilities, the direct medical cost represents the amount paid by TRICARE. This variable, tracked in the patient's medical record, has been used to estimate the total cost of each medical encounter in other reports evaluating medical costs for soldiers in the MHS.4–6
To determine the total direct medical cost, all hospital admission and outpatient encounter records with a heat exhaustion or heat stroke diagnosis meeting inclusion criteria were examined and the full cost and/or total amount paid for each heat illness encounter were summed by soldier and the date of care. Total direct medical care cost includes the cost of care associated with follow-up visits. The heat illness type was assigned based on the ICD-10 code in the primary or secondary position. The record was designated a heat stroke when either of the fields had a heat stroke diagnosis. Data were reported by clinical setting (outpatient and inpatient) and by heat illness type (heat exhaustion and heat stroke).
Results
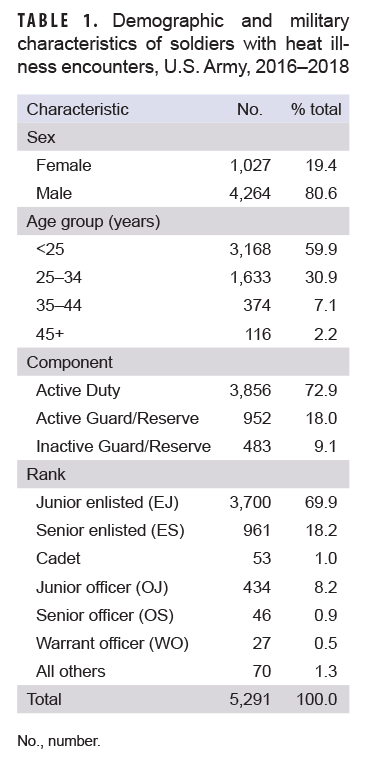
During the study period, 5,291 soldiers—1,027 (19.4%) females and 4,264 (80.6%) males—had 1 or more clinical records associated with heat stroke or heat exhaustion events (Table 1). The majority were enlisted soldiers (88.1%) and younger than 35 years old (90.8%). Of the soldiers who received care for a heat illness, 1 in 4 were members of the National Guard/Reserve.
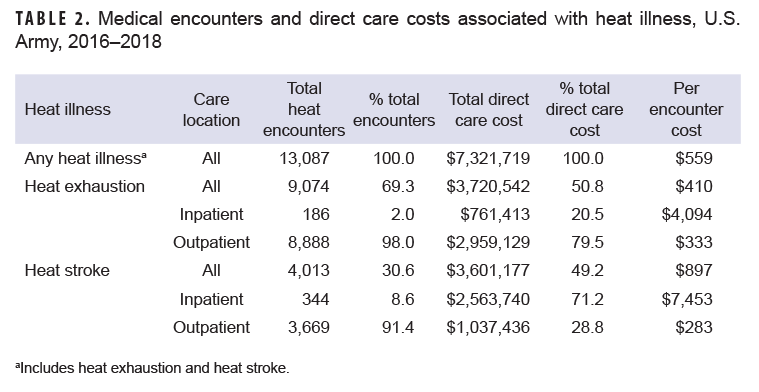
The 5,291 soldiers had 13,087 records of encounters for heat illnesses that resulted in an average of 2.5 medical encounters per soldier (Table 2). The majority of the soldiers' records indicated heat exhaustion diagnoses (69.3%), of which 98.0% were recorded during outpatient encounters. Similarly, 91.4% of heat stroke diagnoses were made during outpatient encounters. The number of heat stroke admissions was nearly double that of heat exhaustion; the number of hospital bed days associated with heat stroke admissions (786 bed days) was 3 times the number associated with heat exhaustion admissions (263 bed days) (data not shown).
The total Click to closeDirect CareDirect care refers to military hospitals and clinics, also known as “military treatment facilities” and “MTFs.”direct care cost to the Army for heat stroke and heat exhaustion encounters was $7.3 million, or $559 per encounter. Even though approximately 70% of the medical encounters were related to heat exhaustion, cost was almost evenly divided between heat exhaustion and heat stroke encounters ($3.7 million and $3.6 million, respectively). The total cost of outpatient encounters was approximately 20% higher than the cost of inpatient admissions ($3.9 million and $3.3 million, respectively). An inpatient heat stroke encounter ($7,453/encounter) was more than 10-fold as costly as the aggregate cost per encounter ($559/encounter).
Editorial Comment
This is the first report in the literature summarizing the direct medical costs associated with heat illness diagnoses among U.S. Army soldiers. A major strength of this study is its inclusion of all active Army and active and inactive National Guard/Reserve soldiers diagnosed with heat illnesses in outpatient and inpatient settings at both military treatment and civilian facilities. For example, in 2015, DeGroot and colleagues7 found an overall treatment cost of $408,074 for heat injuries occurring among 128 of the 10,580 soldiers attending Army Ranger School, which is held at 1 military installation. The DeGroot and colleagues study, which included only Army Ranger trainees, found that the cost per encounter for heat exhaustion treated at the Ranger aid station ranged from $176 to $216 per encounter. The authors estimated that the cost per encounter ranged from $3,024 to $4,327 for heat exhaustion treated but not admitted to a hospital (outpatient), while the cost of an encounter for heat stroke, as indicated by a hospital admission (inpatient), ranged from $5,000 to $6,878 per encounter.7 Using more precise encounter and hospitalization data from 5,291 U.S. Army soldiers with a heat injury over a 3-year period, the current study found a total direct care cost of $7,321,719 for heat injuries. The cost per encounter was $410 for heat exhaustion and $897 per heat stroke encounter.
Direct medical costs are only a portion of the total cost associated with heat illness. Indirect costs of illness account for costs associated with absenteeism, lost productivity, and decreased performance.8–10 In the military, there are lost productivity costs to the Army in the form of 1) lost duty days (or absenteeism), where the soldier is paid but is not able to perform the relevant duties because of health-related reasons, such as hospitalization, and 2) limited duty days, in which a soldier performs the relevant duties but at diminished capacity following an illness or injury.4,6 This analysis notes a total of 1,049 bed days (or lost duty days) due to heat illness diagnoses. Based on average soldier pay for the study timeframe and assuming the loss of 8 hours per day, these lost duty days total $356,000 in lost cost to the Army.
While data for medical profiles associated with heat illness were not available, the indirect costs of the lost and limited duty time associated with medical profiles have been estimated at almost 80% of the total cost of other injuries.4,6 If we assume this cost ratio for heat illness, indirect costs could reach $36 million. A future analysis should incorporate lost and/or limited duty heat illness profile data in order to provide a better estimate of the total cost of these conditions to the Army.
There were 2 main limitations to the study. The surveillance period for this report covered the period 1 Jan. 2016 through 31 Dec. 2018, so it is possible that some initial costs occurring before Jan. 2016 and some follow-up and sequelae visits occurring after Dec. 2018 were not accounted for in the full care cost for each heat illness event. Additionally, the cost assigned by the MHS to heat injury as a primary diagnosis reflects the intensity and complexity of care for other illnesses or injuries (e.g., gastroenteritis, stress fracture) that may be present at the time of the encounter.11
Author affiliations: Armed Forces Health Surveillance Branch, Silver Spring, MD (Dr. Forrest, Dr. Maule, Ms. McCabe, Ms. Kebisek, Mr. Steelman, and Dr. Ambrose).
Disclaimer: The contents, views, or opinions expressed in this publication are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency or the Department of Defense.
References
- Armed Forces Health Surveillance Branch. Surveillance Case Definition. Heat illness. https://health.mil/Reference-Center/Publications/2019/10/01/Heat-Injuries. Accessed 20 Feb. 2020.
- Armed Forces Health Surveillance Branch. Update: Heat injures, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(4):15–20.
- Barnes SR, Ambrose JF, Maule AL, et al. Incidence, timing, and seasonal patterns of heat illnesses during U.S. Army basic combat training, 2014–2018. MSMR. 2019;26(4):7–14.
- Hauschild VD, Lee T, Barnes S, Forrest L, Hauret K, Jones BH. The etiology of injuries in US Army initial entry training. US Army Med Dep J. 2018;(2-18):22–29.
- Bulzacchelli MT, Sulsky SI, Zhu L, Brandt S, Barenberg A. The cost of basic training injuries in the U.S. Army: injury-related medical care and risk factors. Final Technical Report. Fort Belvoir, VA: Defense Technical Information Center.
- Hauschild VD, Forrest LJ, Hirleman C, Pinyan EC, Grier T, Jones BH. Pectoralis major injuries in the Army, CY 2016 active duty Army. APHC PHIP No. 12-03-0719. Public Health Information Paper. Fort Belvoir, VA: Defense Technical Information Center.
- DeGroot DW, Kenefick RW, Sawka MN. Impact of arm immersion cooling during Ranger training on exertional heat illness and treatment costs. Mil Med. 2015;180(11):1178–1183.
- Johns G. Presenteeism in the workplace: a review and research agenda. J Organ Behav. 2010;31(4):519–542.
- Mitchell RJ, Bates P. Measuring health-related productivity loss. Popul Health Manag. 2011;14(2):93–98.
- Rice DP, Hodgson TA, Kopstein AN. The economic costs of illness: a replication and update. Health Care Financ Rev. 1985;7(1):61–80.
- Defense Health Agency. Uniform Business Office User Guide. May 2018. https://health.mil/Reference-Center/Reports/2018/09/27/DHA-UBO-User-Guide-May-2018. Accessed 14 April 2020.