What Are the New Findings?
The prevalence of fibromyalgia (FM) among the active component of the U.S. Armed Forces has not been evaluated since the change from ICD-9 to ICD-10 diagnosis coding, which allows for more accurate capture of FM diagnoses. The estimated prevalence of FM was 0.15% in calendar year 2018.
What Is the Impact on Readiness and Force Health Protection?
Although the prevalence of FM was low in this study population, the high number of health care encounters per affected individual constitute a relatively large burden of disease. The average number of encounters per patient per year was 57 (range=1–263). This clearly presents a significant concern for the readiness and performance of these patients.
Abstract
This report uses routinely collected data in the Defense Medical Surveillance System (DMSS) to characterize the prevalence and burden of fibromyalgia (FM) among members of the active component of the U.S. Armed Forces of FM was 0.15%. There was a trend of increasing prevalence with increasing age. Prevalence was highest among women (0.59%), those in the oldest age group (0.52%), non-Hispanic blacks (0.25%), those in the Air Force (0.21%), those in a health care occupation (0.36%), senior enlisted (0.24%) and warrant officers (0.24%). The prevalence of FM was approximately twice as high among non-Hispanic blacks compared to non-Hispanic whites. The average number of medical encounters per FM patient per year was 57 (median 38, LQ=21, UQ=66, range=1–263) compared to an average of 13 in the total patient population. The groups of conditions most commonly associated with an FM diagnosis were musculoskeletal and mental health conditions. The burden of FM disease poses clear readiness and retention concerns.
Background
Fibromyalgia (FM) is a common cause of widespread musculoskeletal pain.1 The American College of Rheumatology (ACR) created diagnostic criteria for Widespread Pain Index and symptom severity scale.2 In order for a diagnosis of FM to be made a syndrome of focal areas of pain, not explainable by other conditions, must be present in at least 4 of 5 regions of the body and must have been present for at least 3 months, potentially including other somatic symptoms.2 FM is present in 1.75% of the civilian population according to data from the 2012 National Health Interview Survey.3 Walitt et al. found that FM occurred predominantly in women, beginning in the second decade of life, increased with age, and had similar prevalence by race with the exception of a lower prevalence in Asians.3 These findings are consistent with the results of several studies of FM prevalence in the U.S.1,3,4
Patients with an FM diagnosis have comorbid conditions at 1.45 times the rate of those without an FM diagnosis.5 Mental disorders, diseases of the musculoskeletal system, and painful neuropathic disorders among other comorbid conditions occur frequently in FM patients.6 FM can be a prolonged and debilitating condition that is difficult to manage, especially given its association with increased comorbidities.5 The severity and frequency of symptoms can make employment difficult for those with FM.7
In a 2008 study, White and colleagues found that the prevalence of disability was approximately twice as high in patients with FM compared to their peers without FM.7 FM patients in the White et al. study missed an average of 30 days of work per year.7 Patients with FM are often frequent consumers of health care services, utilizing care at a rate 5 times that of the insured U.S. population and averaging up to 6.9 visits per 3-month period.8 Absenteeism and presenteeism (the concept of reduced performance at work due a specific cause) are important to consider as well. Chandran and colleagues found that up to 20% of FM patients reported missing 5 or more days of work in the past month.8 Patients in this study also reported that up to 252 days of work per year were adversely affected by FM.8
Results of a 2017 study of women veterans suggested that exposure to environmental, physical, and psychological stressors associated with military and combat duty increased the risk of developing FM in this population.9 Prevalence of FM among U.S. military members was last formally assessed in a 2014 study that reported an increasing prevalence of FM from 0.31% in 2006 to 0.52% in 2010.10 However, this study estimated FM prevalence among all TRICARE beneficiaries, not just active component service members and relied on the nonspecific International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for FM (729.1, myalgia and myositis, unspecified). Using this code likely resulted in inflated counts of FM diagnoses because active component personnel typically experience muscle strain at rates higher than the general population. The current study describes the prevalence of FM in active component service members and the corresponding burden on FM patients and the Military Health System (MHS).
Methods
The surveillance period was from 1 Jan. 2018 through 31 Dec. 2018. The surveillance population included all individuals who served in the active component of the U.S. Army, Navy, Air Force, or Marine Corps. All data used in this analysis were derived from records routinely maintained in the Defense Medical Surveillance System (DMSS). These records capture information from care received in military and civilian treatment facilities so long as they were reimbursed through the MHS.
For this study, a case was defined as an active component service member with at least 1 inpatient hospitalization during 2018 for which the DMSS record showed a diagnosis for FM (ICD-10 M79.7) in any diagnostic position or at least 2 outpatient visits within 365 days (at least one of the encounters must have been in 2018) with FM diagnosed in any diagnostic position. Prevalence was calculated by dividing the total number of unique individuals meeting the preceding criteria by the population at the midpoint of the year. Mid-year population was used because the active component of the armed forces is an open population with members entering and leaving throughout the year. The following demographic information was captured for each patient at mid-year: age, sex, race/ethnicity group, branch of service, rank, and military occupation.
The numbers of hospitalizations, bed days, and outpatient encounters were totaled for all individuals diagnosed with FM in 2018 to quantify the burden of FM. For this FM burden calculation, the inpatient or outpatient encounter must have had a diagnosis of FM in the first diagnostic position. Only one encounter per patient per day was counted with priority given to inpatient encounters.
The burden of illness and injury comorbidities among the prevalent cases of FM was tabulated in accordance with previously published methodology used for the MSMR burden of disease reports.11 For those who met the case definition for FM, all illness and injury diagnoses recorded in the first diagnostic position of an inpatient or outpatient encounter during calendar year 2018 were ascertained. These encounters were then grouped into 25 burden of disease major categories based on a modified version of the Global Burden of Disease Study.12 Again, only one encounter per patient per day was included in the analysis. These comorbid diagnoses were also grouped by the 17 ICD10 chapters with the 5 most frequently diagnosed conditions reported for each chapter.
Results
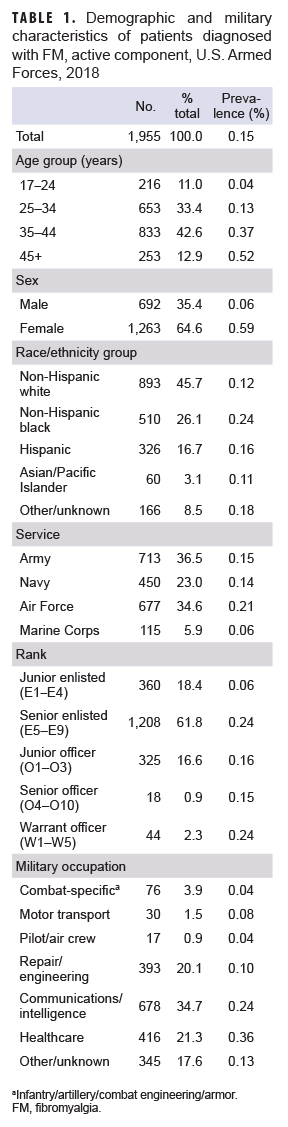
In 2018, a total of 1,955 active component service members met the case definition for FM. This count of cases represents a total prevalence of 0.15% (Table 1). Prevalence increased linearly with age from 0.042% in the 17-24 age group to 0.52% in the 45+ age group. FM was 9.29 times more common in women than men. The prevalence of FM in non-Hispanic blacks (0.245%) was 2 times higher than that in the non-Hispanic white (0.12%) population, and prevalence was very similar between whites and Asian/Pacific Islanders (0.11%). FM was most common in the Air Force (0.21%) and least common in the Marine Corps (0.06%). Senior enlisted and warrant officers were diagnosed with FM at similar levels (both 0.24%), while junior enlisted had the lowest levels (0.06%). Communications/intelligence and health care personnel had the greatest prevalence of FM diagnosis compared to other occupational groups (0.24% and 0.36%, respectively), while combat-specific occupations had a relatively low prevalence of 0.04% (Table 1).
In 2018, there was 1 inpatient encounter with the ICD-10 code for FM in the first diagnostic position. Other diagnosis codes listed in the discharge summary for this admission included eosinophilia, abdominal pain, constipation, and leaving against medical advice. There were 6,801 outpatient encounters with FM in the first diagnostic position among 1,535 individual patients meeting criteria to be considered a patient with FM in this study (data not shown). This represents an average of 4.4 outpatient encounters attributable to FM per patient with FM per year. Patients with FM had an average of 57 medical encounters per year (median 38, LQ = 21, UQ = 66, range=1–263) (data not shown). The MSMR burden of disease report for the same year found that all active component service members had an average of 13 encounters per year.
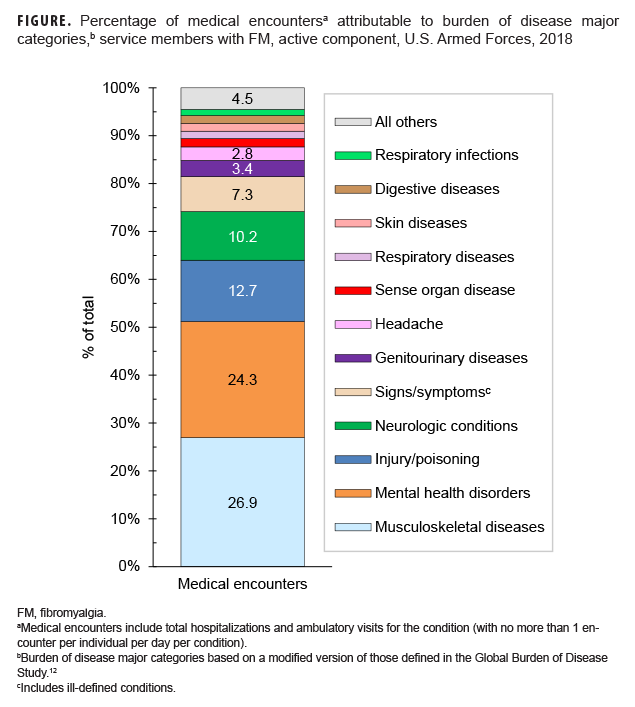
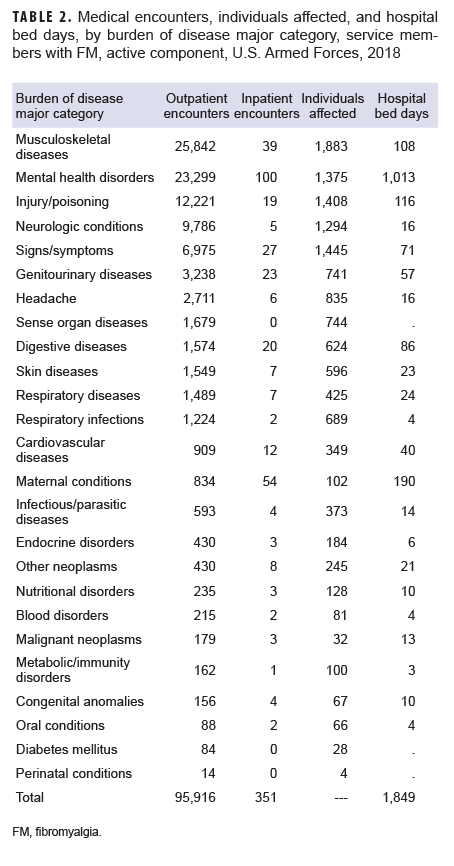
Encounters for comorbid conditions were counted for all 1,955 prevalent cases of FM. The 5 MSMR burden of disease major categories of diagnoses with the most encounters among the 1,955 FM cases in 2018 were musculoskeletal diseases (26.9% of all encounters), mental health disorders (24.3%), injury/poisoning (12.7%), neurologic conditions (10.2%), and signs, symptoms and ill-defined conditions (7.3%) (Figure 1). These 5 burden of disease major categories accounted for 81.4% of all FM patient encounters in 2018. Among patients with FM, nearly all (96.3%; n=1883) had an encounter for a musculoskeletal disease (Table 2), accounting for 25,842 encounters. Within the major category of musculoskeletal disease, the two most common sub-categories were 'all other musculoskeletal diseases' (n=14,099), and 'other back problems' (n = 10,920) (data not shown). The sub-category 'all other musculoskeletal diseases' included the diagnosis of FM. Within the mental health disorders (n=23,299) category, the two most common sub-categories were anxiety disorders (n=9,421) and mood disorders (n=6,904). The two most common sub-categories within injury/poisoning (n=12,221) were arm and shoulder injuries (n=3,464) and knee injuries (n=2,333). Within neurologic conditions (n=9,786) the 2 most common sub-categories were organic sleep disorders (n=5,382) and 'all other neurologic conditions' (n=4,144) (excluding epilepsy, multiple sclerosis, and mononeuritis). Lastly, within signs and symptoms (n=6,975) the 2 most common sub-categories were 'abdomen and pelvis' (n=1,405) and 'all other signs and symptoms' (n=4,414) (excluding the only other category, 'respiratory and chest' (n=1,183)) (data not shown).
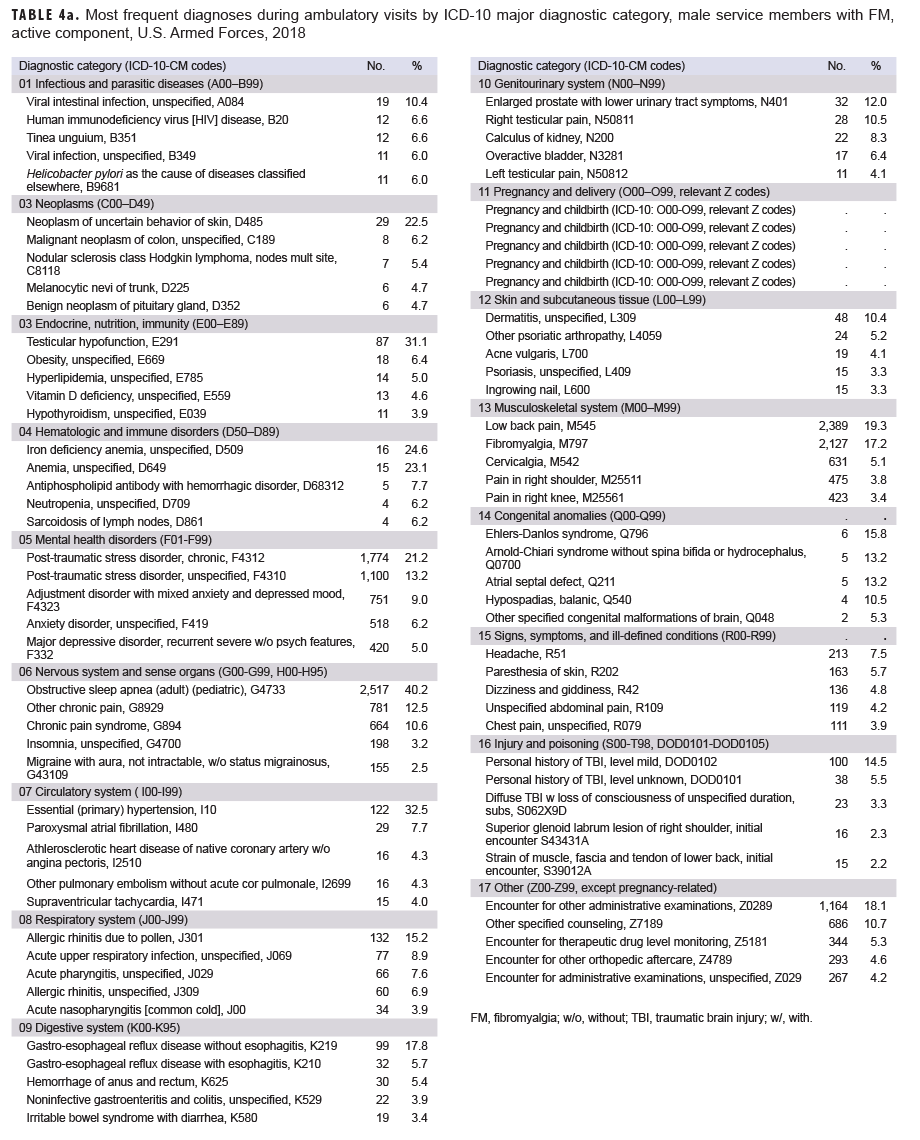
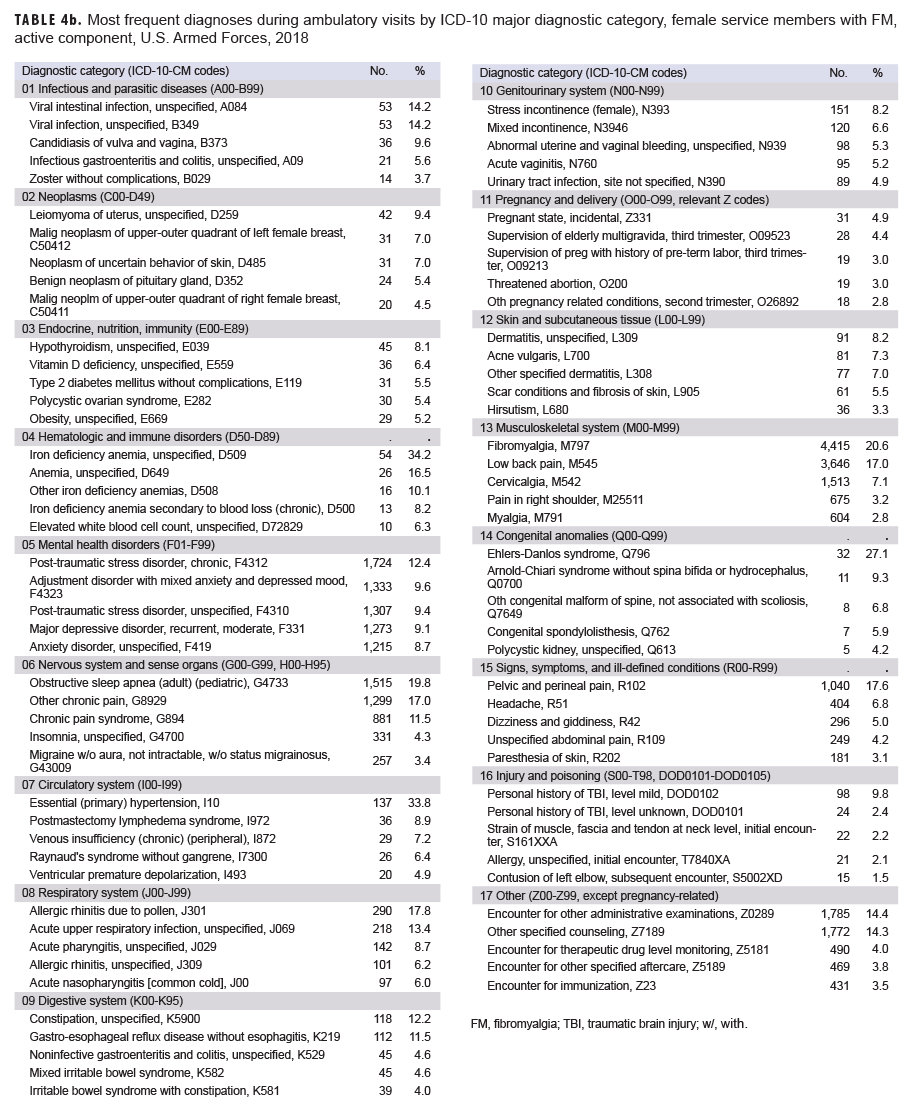
Outpatient encounters were also quantified according to ICD-10 chapters and specific ICD-10 diagnostic codes (Table 3, 4a, and 4b). The distribution of diagnoses was broadly similar for men and women. The top 5 comorbid diagnoses by ICD-10 major diagnostic category for FM patients were for musculoskeletal system disorders (30.5%), mental health disorders (20.1%), factors influencing health status and contact with health services (17.0%), disorders of the nervous system and sense organs (12.6%), and signs, symptoms, and ill-defined conditions (7.9%) (Table 3).The 2 most common diagnoses within the musculoskeletal system chapter were fibromyalgia and low back pain, comprising 19.4% and 17.9% of all musculoskeletal system primary diagnoses, respectively. Within the mental health disorders category, post-traumatic stress disorder (PTSD) and adjustment disorder were the 2 most common diagnoses accounting for 26.5% and 9.4% of mental health disorder-related outpatient encounters, respectively (Tables 4a, 4b). Among nervous system and sense organ diagnoses obstructive sleep apnea and chronic pain were the most common with 29.0% and 26.1% of encounters, respectively. Lastly, within the signs, symptoms, and ill-defined conditions chapter, pelvic and perineal pain accounted for 11.7% of visits and headache accounted for 7.1% of visits.
Editorial Comment
The period prevalence of FM in the active component of the U.S. armed forces was found to be 0.15% in 2018 based on diagnoses made in medical encounters. Prevalence in the U.S. was 1.75% based on diagnoses made via modified ACR criteria based on responses to the 2012 National Health Interview Survey.3 Jeffery et al. found a prevalence of 0.52% in 2010 among all TRICARE beneficiaries including active duty, dependents, and retirees.10 The Jeffery et al. study utilized the ICD-9 code 'myalgia and myositis, unspecified' which they acknowledge likely misclassified the outcome by including additional conditions such as myalgia, a common diagnosis for the active component.10
The marked difference in the prevalence estimate from the current analysis (0.15%) and that reported by Walitt et al. (1.75%) is likely partially explained by differences in methodology. In the Walitt et al. study, only 27% of respondents diagnosed with FM via the survey reported having the FM diagnosis. Applying this percentage to their reported prevalence yields a prevalence of formally diagnosed FM of 0.47%. The remaining difference may be partially explained by the healthy worker effect, the younger age of the active component population, and/or the disincentive for seeking care among active component service members (e.g., loss of flight privileges).
The Armed Forces have strict retention criteria, which may have also contributed to the low prevalence observed in this study. For example, the Air Force Medical Standards Directory states that patients with "fibromyalgia requiring regular use of controlled medications, schedule II-IV, or requiring frequent follow up or duty restrictions" are not qualified for retention.13 The document does not define the frequency of follow up. Similar language is present in the Department of Defense Instruction 6490.07 and DoD Instruction 1332.45 (Deployment Limiting Medical Conditions for Service Members and DoD Civilian Employees and Retention Determinations for Non-Deployable Service Members respectively).14,15 Patients with FM within the active component had an average of 4.4 FM-related outpatient encounters and 57 total medical encounters per year. These counts represent a 3 to 4-fold increase above those seen in the total active component. Such levels of health care utilization may result in those with FM not being retained in the Armed Forces, contributing to a lower prevalence. Such personnel losses represent a significant amount of time and impact on readiness.
The trend of increasing prevalence with age in the active component is similar to that seen in the U.S. civilian population.3 In addition, the difference in prevalence between men and women (1:9) is similar to that reported in the published literature.1,3-7 More senior ranks had greater prevalence consistent with the age trend, but senior officers were the exception. This finding may represent some protective feature of this population or it may be that men comprise a greater portion of the senior officer population. Individuals in health care occupations had the greatest prevalence of FM. This observation may be explained by the comparative ease of making/keeping appointments, reduced stigma surrounding FM in a health care setting, or increased awareness of the condition. Prevalence in non-Hispanic Blacks was more than twice as high as that in non-Hispanic Whites. This relationship was not evident in the literature reviewed. It may be that non Hispanic Blacks experience barriers to care, and thus barriers to diagnosis/capture, in the civilian population, whereas, this effect may not be present in the military health system due to universal access to care. There is no clear explanation of this finding in the data, so this is a topic that deserves future research.
There is a marked difference in the distribution of mental health diagnoses between the FM patient population and the total active component (as described in the annual MSMR burden of disease reports11). Mental health diagnoses comprise twice the percentage of encounters in the FM population compared to the total active component. In 2018, PTSD accounted for more than a quarter of the encounters among active component service members affected by FM which is double the proportion in the total active component population in the same year. These data support existing theory that emotional stress can precipitate or exacerbate FM.16 These comorbidities pose a substantial burden to the readiness of these patients.
The limitations of this study include potential misclassification bias due to the case definition for FM. Patients who had FM but did not have an encounter with FM as a diagnosis in 2018 were not included in the prevalence estimate. Those who were being ruled out for FM may have been included in the prevalence estimate despite not truly having FM. This was a study of the active component of the U.S. Armed Forces and thus has limited generalizability outside of this population. This was a cross-sectional study without evaluation of an exposure of interest.
This study established the prevalence and burden of FM in the active component as well as the burden of comorbidities among patients with FM. FM requiring frequent follow up is grounds for a medical evaluation board and subsequent separation. This was a cross-sectional study and thus did not provide longitudinal data. A future study in which a cohort of patients with FM were followed would be useful in addressing several knowledge gaps. Such a study could assess whether patients with FM are receiving standard of care, if the frequency of encounters related to the quality of care, and which patients are medically separated. Answers to these questions would give actionable information regarding the FM patient population.
Author affiliations: Madigan Army Medical Center, Joint Base Lewis-McChord, WA (Maj Hulse); Armed Forces Health Surveillance Division, Silver Spring, MD (Dr. Stahlman, Ms. Fedgo, Dr. Beason Serafica, and CDR Clausen).
Disclaimer: The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, assertions, opinions, or policies of the Uniformed Services University of the Health Sciences (USUHS), the Department of Defense (DoD), or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
References
- Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38(1):19–28.
- Wolfe F, Clauw DJ, Fitzcharles M, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016; 46(3):319–329.
- Walitt B, Nahin RL, Katz RS, Bergman MJ, Wolfe F. The prevalence and characteristics of fibromyalgia in the 2012 National Health Interview Survey. PloS One. 2015;10(9): e0138024.
- Heidari F, Afshari M, Moosazadeh M. Prevalence of fibromyalgia in general population and patients, a systematic review and meta-analysis. Rheumatol Int. 2017;37(9): 1527–1539.
- Berger A, Sadosky A, Dukes EM, Edelsberg J, Zlateva G, Oster G. Patterns of health care utilization and cost in patients with newly diagnosed fibromyalgia. Am J Manag Care. 2010;16(5 Suppl):S126–S137.
- Lachaine J, Beauchemin, Landry PA. Clinical and economic characteristics of patients with fibromyalgia syndrome. Clin J Pain. 2010;26(4):284–290.
- White LA, Birnbaum HG, Kaltenboeck A, Tang J, Mallett D, Robinson RL. Employees with fibromyalgia: medical comorbidity, health care costs, and work loss. J Occup Environ Med. 2008;50(1):13–24.
- Chandran A, Schaefer C, Ryan K, Baik R, McNett M, Zlateva G. The comparative economic burden of mild, moderate, and severe fibromyalgia: results from a retrospective chart review and crosssectional survey of working-age US adults. J Mang Care Pharm. 2012;18(6):415–426.
- D'Aoust RF, Rossiter AG, Elliott A, Ji M, Lengacher C, Groer M. Women veterans, a population at risk for fibromyalgia: The associations between fibromyalgia, symptoms, and quality of life. Mil Med. 2017;182(7):e1828–e1835.
- Jeffery DD, Bulathsinhala L., Kroc M, Dorris J. Prevalence, health care utilization, and costs of fibromyalgia, irritable bowel, and chronic fatigue syndromes in the military health system, 2006–2010. Mil Med. 2014;179(9):1021–1029.
- Armed Forces Health Surveillance Branch. Ambulatory visits, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):19–25.
- Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press, 1996:120–122.
- Department of the Air Force. U.S. Air Force Medical Standards Directory. Approved by AF SG3C. 13 May 2020.
- Department of Defense. Instruction 6490.07, Deployment-Limiting Medical Conditions for Service Members and DOD Civilian Employees. 5 February 2010.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 1332.45, Retention Determinations forNon-Deployable Service Members. 30 July 2018.
- Sluka KA, Clauw DJ. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience. 2016;338:114–129.