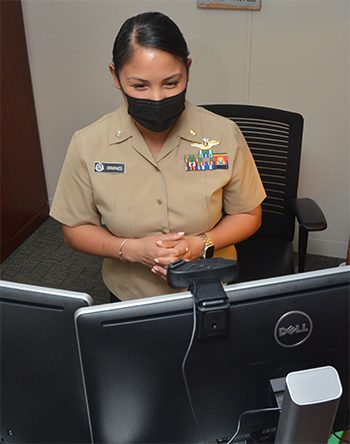
 Navy Cmdr. Hannah Starnes, director of mental health at Naval Hospital Jacksonville, and her staff adapted to the COVID-19 pandemic by expanding telehealth options, counting more than 33,000 enrollees since the onset of the pandemic. (Photo courtesy of Naval Hospital Jacksonville.)
Navy Cmdr. Hannah Starnes, director of mental health at Naval Hospital Jacksonville, and her staff adapted to the COVID-19 pandemic by expanding telehealth options, counting more than 33,000 enrollees since the onset of the pandemic. (Photo courtesy of Naval Hospital Jacksonville.)
“We had to think of new ways to keep people safe and still offer the health care they needed,” she said. “Specifically, for my section, I had to think of ways to schedule personnel to accomplish the work and keep them safe and distant from one another.
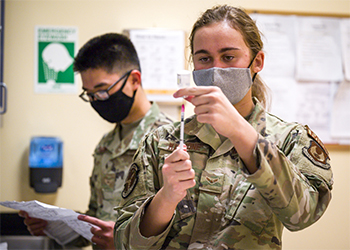
Another aspect, she said, was preparing for the mass testing we were expected to perform for COVID-19. “We were one of the first labs to have the Centers for Disease Control and Prevention’s COVID-19 testing in place during the beginning of the pandemic.”
Navy Cmdr. Hannah Starnes agreed. As the director of mental health at the Navy Medicine Readiness and Training Command Jacksonville, Florida, she and her team had to think “really creatively” to leverage technology and continue taking care of their patients, particularly active-duty service members.
“There were a lot of technological changes that we had to make,” she said. “We utilized our command’s virtual video solution to allow our patients to access our providers from home, through an encrypted, safe telehealth solution.”
She explained mental health was already on the forefront of utilizing telehealth even before the pandemic because it allows for easier clinical visits than other medical treatments. The pandemic simply pushed them to leverage it quicker and more widely.
“Several of our providers were already piloting the telehealth program,” she said. “By the time COVID-19 hit, we offered this option to all of the providers, resulting in approximately 95% utilizing that solution by the time April or May 2020 rolled around.”
In the case of emergency management at Walter Reed National Military Medical Center, in Bethesda, Maryland, COVID-19 caused significant changes in the way daily operations were conducted, said Chris Gillette, the center’s command emergency manager.
“Initially, the most notable changes focused on implementing additional safety and security measures for our staff, patients, and visitors,” he said. “Those consisted of establishing controlled access to the hospital, a centralized screening and testing area, strict personal protective equipment and infection control protocols for our staff, and social distancing policies.”
 Air Force Staff Sgt. Tyler Byrd, NCOIC, Immunology, and Air Force Technical Sgt. Jennifer Weigl, NCOIC, Microbiology, prepare patient samples for COVID-19 extraction at Brooke Army Medical Center, Fort Sam Houston, Texas, June 1, 2020. BAMC laboratory technicians are completing COVID tests of all samples taken from patients at BAMC and its neighboring communities. (U.S. Air Force photo by Senior Master Sgt. Sarah Hanaway, Brooke Army Medical Center)
Air Force Staff Sgt. Tyler Byrd, NCOIC, Immunology, and Air Force Technical Sgt. Jennifer Weigl, NCOIC, Microbiology, prepare patient samples for COVID-19 extraction at Brooke Army Medical Center, Fort Sam Houston, Texas, June 1, 2020. BAMC laboratory technicians are completing COVID tests of all samples taken from patients at BAMC and its neighboring communities. (U.S. Air Force photo by Senior Master Sgt. Sarah Hanaway, Brooke Army Medical Center)
WRNMMC also saw changes in its outpatient service mission from a patient care perspective, according to Gillette. Expanding health care to telehealth played a significant role in those changes.
“Although our clinics and other ancillary services were open, many patients did not want to come into the hospital,” he said. “This led to the need to expand our capabilities for telehealth appointments (which worked very well). We also established a drive-thru pharmacy for our patients which we continue to operate today.”
As important as teamwork is in achieving any mission, during the COVID-19 pandemic it was paramount for MHS readiness. Teamwork ensured protocols were established and followed to the letter to avoid interruption of safe, reliable service to beneficiaries in the most trying times.
For Fernandez, the pandemic was the “real test” she and her team had prepared for. Following updated protocols, they were ready “for whatever came their way.”
She credits her leadership for making the difference as DPALS/BAMC undertook testing early in the pandemic.
“This was a massive operation which tested an average of 1,600 test per week,” she said. “Everyone involved knew their role and worked diligently and efficiently to provide results within 24 hours.”
Gillette added that despite the many challenges and rapid changes the pandemic brought on, staff’s professionalism, teamwork, and flexibility were key to adapting to new protocols safely and effectively.
For example, he said, setting up an Incident Response Structure at WRNMMC proved “effective for organizing and coordinating our daily planning efforts, providing clear and consistent policy changes and guidance to our staff and patients, and ensuring a well-executed, coordinated and integrated response,” he said.
In every aspect, the COVID-19 pandemic further proved the MHS’s readiness training is effective during a real-world emergency in which the whole of society must work together.
“It validated the effectiveness of our contingency plans and our ongoing training and exercises designed to maintain continuous ‘all hazards’ readiness,” said Gillette. “This proved to be effective in enhancing operations and our patient care mission.”
Likewise, he said, “the relationships and partnerships we have established over the years with local, state, and federal agencies throughout the region proved highly effective throughout the pandemic.”
“We shared challenges and lessons learned, discussed capabilities and resource needs, and knowing that our neighbors were there to listen and make every effort to offer assistance and support gave everyone a sense of security,” he added.
 Military medical treatment facility staff, like those with the 412th Medical Group at Edwards Air Force Base in California are consistently on the frontlines in the war against the COVID-19 disease. (U.S. Air Force photo by Giancarlo Casem)
Military medical treatment facility staff, like those with the 412th Medical Group at Edwards Air Force Base in California are consistently on the frontlines in the war against the COVID-19 disease. (U.S. Air Force photo by Giancarlo Casem)
According to Starnes, COVID-19 also pushed MHS personnel to think outside the box, thereby becoming more efficient. Since patients were often unable to access their medical treatment facilities in person due to physical distancing safety measures, providers adapted to maintain the active-duty war fighters’ readiness, both by offering telehealth options as well as by maximizing the in-person visits to MTFs patients were able to attend.
“It has really changed our way of managing our patients, almost bringing us back to the basics,” she said. “We’re looking at patients more holistically, considering how we can best maximize and optimize the time we have with them, whether they’re physically in front of us or virtually.”
As an example, she explained that when a patient comes in to the MTF for a specific primary care consult but may also soon be due for other routine or specialty care screening or testing, lab work, or x-rays, the staff at NH Jacksonville tries to maximize the visit by preparing in advance of the patient’s arrival and getting as much as possible done in that visit to avoid them from having to come in again.
In addition, she said having an option for telehealth has been helpful for patients who may be transitioning between duty stations or sailors attached to a ship, who are unable to come into an MTF.
“Telehealth allows their health care not to be gapped during that transition period or when they get off the ship,” said Starnes. “As long as they’re within wi-fi or cell phone coverage, we can still have an appointment with them, at least from the mental health standpoint, and not interfere with their readiness mission.”
That way, “they don’t have to leave for half a day to go to an appointment at the hospital,” she said. “They can still stay in their workplace, have their appointment, and go back to work.”
As proof of the success telehealth has offered, Starnes pointed to the numbers of enrollees in telehealth at Naval Hospital Jacksonville since the COVID-19 pandemic began.
“Prior to COVID, we only had about 6,700 patients enrolled in telehealth, and now we’re over 33,000,” she concluded.