The U.S. Advisory Committee on Immunization Practices recommends vaccination for all health care personnel against influenza to protect both themselves and their patients.1 The Joint Commission’s standard for infection control emphasizes that individuals infected with influenza virus are contagious to others before any signs or symptoms appear. The Joint Commission mandates 90% influenza vaccination for health care personnel, and health care organizations provide influenza vaccination programs for their practitioners and staff. Within the Department of Defense, seasonal influenza immunization is mandatory for all uniformed and health care personnel who provide direct patient care, and is recommended for all others (excluding those medically exempt).2-5
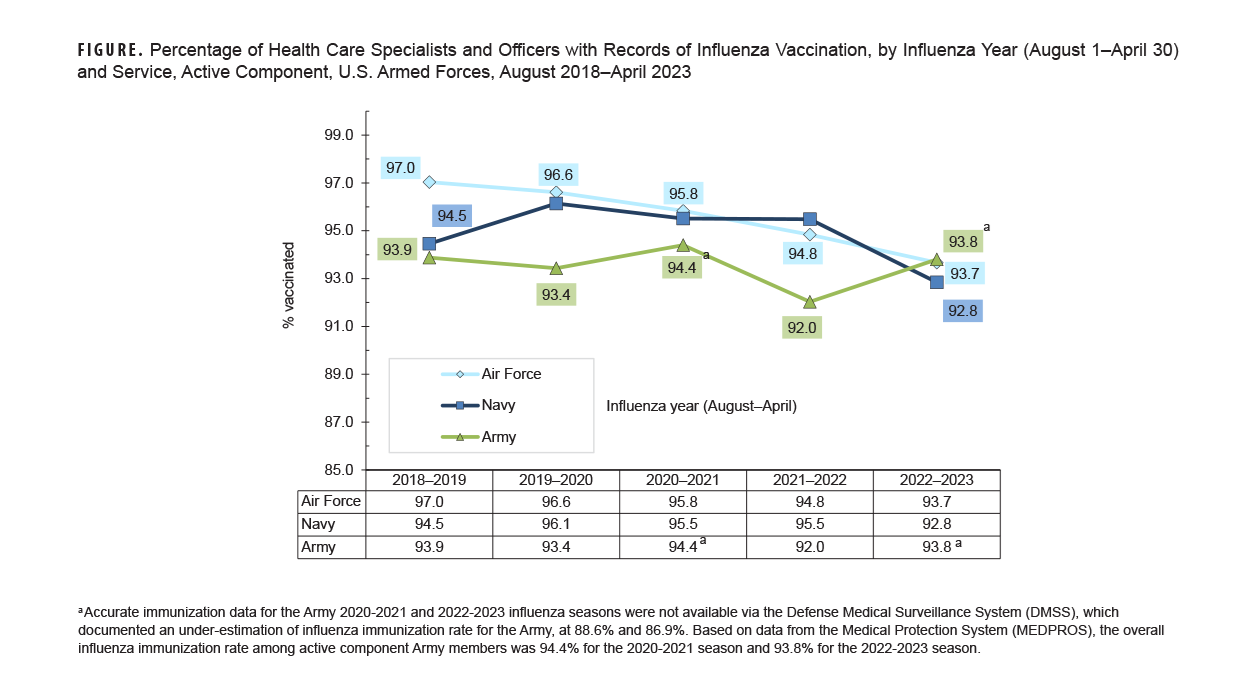
This Surveillance Snapshot covers a 5-year surveillance period (August 2018–April 2023) and presents the documented percentage of compliance for the influenza immunization requirement among active component health care personnel of the Army, Navy, and Air Force. In general, these health care personnel include health care specialists (DOD occupation code=13) and health care officers (DOD ocupation code=26), but exclude veterinary medicine, environmental health, biomedical equipment maintenance and repair, and health services administration and logistics personnel. In the 2022-2023 influenza season, compliance rates ranged from 92.8% among Navy health care personnel to 93.8% among Army health care personnel (Figure).
References
- Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2011;60(RR-7):1-45.
- Headquarters, Departments of the Army, Navy, Air Force, and Coast Guard. Army Regulation 40-562, BUMEDINST 6230.15B, AFI 48-110_IP, CG COMD-TINST M6230.4G. Medical Services: Immunizations and Chemoprophylaxis for the Prevention of Infectious Diseases. Oct. 7, 2013.
- Assistant Secretary of Defense (Health Affairs). Policy for Mandatory Seasonal Influenza Immunization for Civilian Health Care Personnel Who Provide Direct Patient Care in Department of Defense Military Treatment Facilities. Health Affairs Policy 08-005. Apr. 4, 2008.
- Assistant Secretary of Defense (Health Affairs). Addition of Pandemic Influenza Vaccine or Novel Influenza Vaccine to the Policy for Mandatory Seasonal Influenza Immunization for Civilian Health Care Personnel Who Provide Direct Patient Care in Department of Defense Military Treatment Facilities. Health Affairs Policy 11-010. Jul. 28, 2011.
- Defense Health Agency. Procedural Instruction 6025.34. Guidance for the DOD Influenza Vaccination Program. Aug. 21, 2020.