Sunburn affects U.S. military mission readiness, from clothing and gear discomfort, to infection and dehydration risk due to skin barrier breakdown and fluid loss.1 Depending on a service member’s military occupation, ultraviolet radiation exposure will vary, as seen with higher incidences of sunburn in recruits, aircraft and aircraft-related occupations, and infantry.1 Clinically, sunburn is classified and managed within two main categories: mild-moderate and severe.2 Electronic health record sunburn documentation is determined by International Classification of Diseases, 10th Revision diagnosis codes that classify sunburn as sunburn of first degree, second degree, third degree, or unspecified. Sunburn of first degree (superficial burn) only affects the outer layer of the skin (epidermis), manifesting in mild to moderate erythema without blistering. Sunburn of second degree (partial thickness burn) affects both the epidermis and part of the dermis, resulting in erythema with blistering, with or without edema. Sunburn of third degree (full thickness burn) affects the epidermis and dermis, and occasionally the underlying bones, muscles, and tendons.
A significant cause of skin cancer is excessive UVR exposure, often in the form of repeated sunburn.3 Among U.S. military service members, non-melanoma skin cancers are the most frequently diagnosed cancer.4,5 Additionally, a recent Department of Defense report found that U.S. military aircrew had an 87% higher rate of melanoma, and aviation support personnel (ground crew) had a 9% higher rate of melanoma, compared to the general U.S. population.6
A 2014 MSMR report documented 19,172 incident cases of clinically-diagnosed sunburn among active component service members of the U.S. military from January 2002 to December 2013.1 Incidence rates were higher among women, non-Hispanic White service members, and those in younger age groups. Additionally, incidence was also higher for those in the Marine Corps and Army, as well as enlisted members, and recruits.1 This report describes recent frequencies and rates of clinically-diagnosed sunburn among active component service members.
Methods
This retrospective cohort study covered a surveillance period from January 1, 2014 to September 30, 2022 and included all ACSM of the U.S. Army, Air Force, Navy, and Marine Corps. Data were derived from the Defense Medical Surveillance System, which is maintained by the Armed Forces Health Surveillance Division. DMSS documents ambulatory care encounters and hospitalizations in fixed military and civilian (if reimbursed through the Military Health System) treatment facilities worldwide.
Outcome of sunburn was identified through inpatient and outpatient medical encounters containing an ICD-9 code of 692.71 (sunburn of first degree), 692.76 (sunburn of second degree), 692.77 (sunburn of third degree), or an ICD-10 code of L55.0 (sunburn of first degree), L55.1 (sunburn of second degree), L55.2 (sunburn of third degree), or L55.9 (sunburn, unspecified), in the first or second diagnostic position. The transition between ICD-9 and ICD-10 codes, in 2015, occurred during the study’s surveillance period.
An individual was classified as a new case of sunburn if at least 30 days passed since the documentation of a previous sunburn-associated medical encounter. Incidence of sunburn was calculated per 100,000 person-years (p-yrs). Negative binomial regression calculated incidence rate ratios for occupation categories, adjusting for sex, age, and race and ethnicity.
Results
Table 1 provides the total incident case counts and crude incidence rates of clinically-diagnosed sunburn among ACSM during the 9-year surveillance period. Over half of the cases were first degree sunburn (n=6,244; 54.5%), and almost all cases were diagnosed in the ambulatory setting (n=12,029; 99.95%). During the 9-year surveillance period, most, 97.1% (n=11,687), reported cases had only 1 diagnosed sunburn.
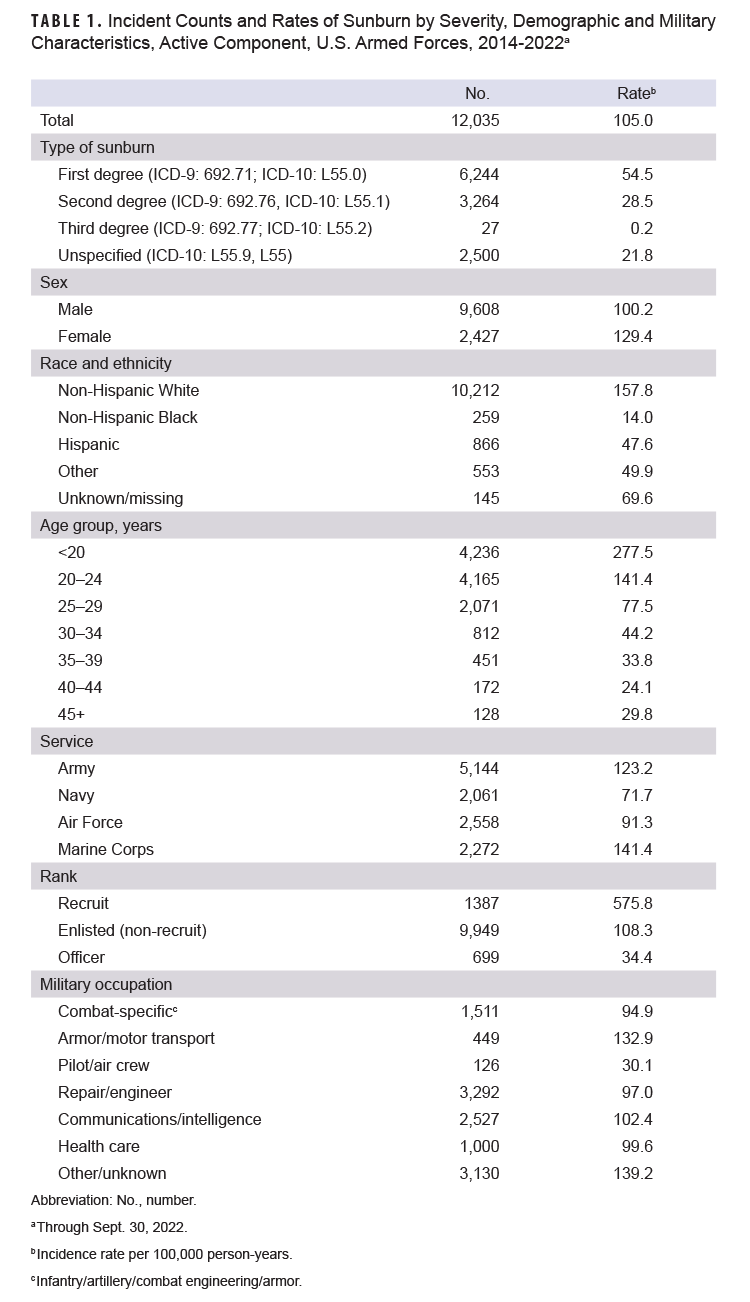
The incidence rate of sunburn diagnosis was higher among women compared to men. Non-Hispanic White service members had the highest rate compared to other races and ethnicities. The three youngest age groups, under 20 years, 20-24, and 25-29 years of age, had the highest incidence rates of sunburn diagnosis, with rates decreasing with increasing age until 45 years of age. The Marine Corps and Army had the highest rates among the services. Recruits had a significantly higher sunburn incidence compared to non-recruit enlisted service members and officers.
The annual total sunburn incidence rates, which varied annually, increased overall 6.4% from 2014 (100.3 per 100,000) through 2022 (106.8 per 100,000). Of the 12,035 cases of sunburn, 5,542 occurred in June (46.0%), more than in any other month (data not shown). Ten military installations/regions accounted for 36% of all sunburns during the surveillance period. The highest overall counts were in Okinawa, Japan (n=513) and San Diego, CA (n=510), followed closely by Fort Moore (formerly Benning), GA (n=468), and Fort Leonard Wood, MO (n=454) (data not shown).
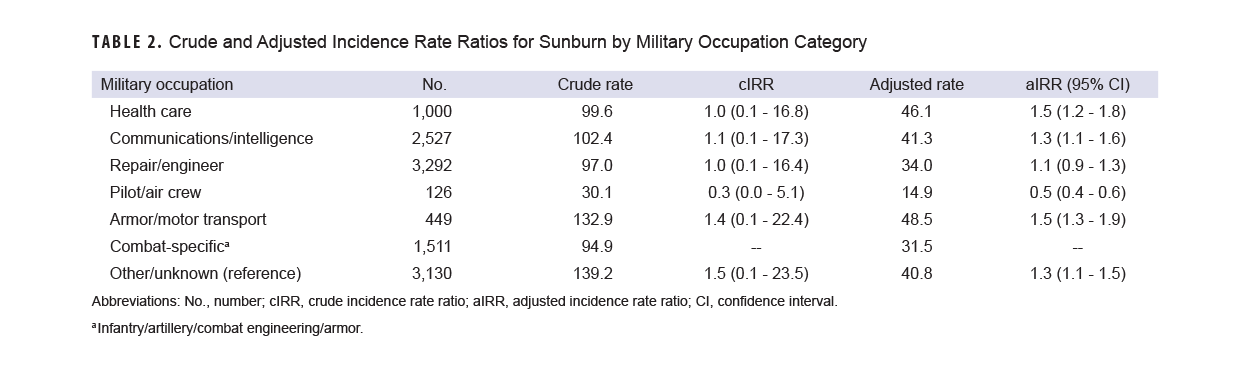
Table 2 provides the crude and adjusted rate ratios for the association between occupational category and sunburn. The pilot/air crew category had the lowest crude and adjusted incidence rate of sunburn diagnosis.
Discussion
Compared to the prior MSMR report, the incidence of clinically-diagnosed sunburn among ACSM decreased 15.9% from 2002-2013 to 2014-2022 (from 124.8 cases per 100,000 p-yrs to 105.0 cases per 100,000 p-yrs).1 In both studies, women demonstrated a higher rate of sunburn diagnosis. Epidemiological data of the general U.S. population suggest that women are less likely to report frequent sunburn and are more likely to implement sunburn prevention measures.7,8,9 According to National Cancer Institute statistics, however, reported sunburn for women differs from men by age, with younger women (aged 18-24) accounting for a higher proportion of sunburns than men in the same age group.10 The majority of ACSM are under 25 years of age, which could partially explain the higher incidence of sunburn among women described in this study.
Similar to the 2014 MSMR report, non-Hispanic White service members and younger age groups had higher diagnosed sunburn rates, which is consistent with the general U.S. population.7 The current study found that pilot/air crew had the lowest rate of sunburn diagnosis, both before and after adjustment for potential confounders, which suggests that other factors such as differences in health care utilization or sunburn prevention measures may influence lower incidence of sunburn diagnoses.
One limitation of this study is outcome misclassification bias for sunburn diagnosis based upon health care utilization. This report likely underestimates the true rate of sunburn, as only individuals with more serious burns are likely to present for medical care. Additionally, the introduction of the ICD-10 code of “unspecified” may limit ascertainment of burn severity, potentially affecting accurate surveillance. A second limitation of this study is that the data could not differentiate sunburn during work hours versus non-work hours, challenging associations of occupation with sunburn risk.
Sunburn affects military readiness by removing service members from duty while their burns heal, affecting both garrison and combat missions. As a risk factor for future skin cancer, sunburn is a longitudinal concern for both the public health sector and the military due to the health care costs and time involved in management of melanoma and NMSC.11,12 Emphasis on prevention should continue.
Sunburn is likely multifactorial, from limited access to sunscreen, to its lack of use, variable encouragement of use by peers or leadership, operational time constraints, and low prioritization or understanding of the long-term effects of sun damage.12,13 Mitigation strategies can include pre-deployment or seasonal health promotion focused on increasing use of available sun-protective measures, including sunscreen, sunglasses, headgear, shade structures, and modified outdoor training times to early morning or later day/early evening.
Survey analysis of military-specific populations could help quantify incidence of sunburn that is more specific than clinical diagnoses, and could quantify occurrence of unreported sunburn. Survey research could evaluate behavioral practices, such as use of preventive measures, location and timing (on- or off-duty) of sunburn, and inquiry about unreported burns, which may better inform sunburn-reduction strategies.
Author Affiliations
Uniformed Services University of the Health Sciences, Bethesda, MD: LT Van Airsdale; Defense Health Agency, Armed Forces Health Surveillance Division: Dr. Stahlman, Ms. Hiban, CAPT Wells.
Disclaimer
The opinions and assertions expressed herein are those of the authors and do not reflect the official policy nor position of the Uniformed Services University of the Health Sciences or the Department of Defense. LT Van Airsdale is a military service member. This work was prepared as part of official duties. Title 17, U.S.C., §105 provides that copyright protection under this title is not available for any work of the U.S. Government. Title 17, U.S.C., §101 defines a U.S. Government work as a work prepared by a military Service member or employee of the U.S. Government as part of that person’s official duties.
References
- Armed Forces Health Surveillance Branch. Sunburn among active component service members, U.S. Armed Forces, 2002–2013. MSMR. 2014;21(7):2-6.
- Young AR and Tewari A. Sunburn. UpToDate. Updated Aug. 4, 2022. Accessed Oct. 10, 2023. https://www.uptodate.com/contents/sunburn
- Guerra KC, Crane JS. Sunburn. In: StatPearls. StatPearls Publishing; 2023. Accessed Apr. 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK534837
- Lee T, Taubman SB, Williams VF. Incident diagnoses of non-melanoma skin cancer, active component, U.S. Armed Forces, 2005-2014. MSMR. 2016;23(12):2-6.
- Mabila S, Dreyer E. Surveillance snapshot: the top 10 incident cancers among active component service members, 2018-2022. MSMR. 2023;30(9):17.
- U.S. Department of Defense. Phase 1-a—Study on the Incidence of Cancer Diagnosis and Mortality Among Military Aviators and Aviation Support Personnel. Jan. 2023.
- Braun HA, Adler CH, Goodman M, Yeung H. Sunburn frequency and risk and protective factors: a cross-sectional survey. Dermatol Online J. 2021;27(4).
- McKenzie C, Nahm WJ, Kearney CA, Zampella JG. Sun-protective behaviors and sunburn among US adults. Arch Dermatol Res. 2023:1-10. doi:10.1007/s00403-023-02547-z
- Reuter NP, Bower M, Scoggins CR, Martin RC, McMasters KM, Chagpar AB. The lower incidence of melanoma in women may be related to increased preventative behaviors. Am J Surg. 2010;200(6):765-769. doi:10.1016/j.amjsurg.2010.06.007
- National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services. Cancer Trends Progress Report/Sunburn. Updated Aug. 2023. Accessed Oct. 13, 2023. https://progressreport.cancer.gov/prevention/sunburn
- Kao SYZ, Ekwueme DU, Holman DM, et al. Economic burden of skin cancer treatment in the USA: an analysis of the Medical Expenditure Panel Survey Data, 2012–2018. Cancer Causes Control. 2023;34:205-212. doi:10.1007/s10552-022-01644-0
- Rosenberg A, Cho S. We can do better at protecting our service members from skin cancer. Mil Med. 2022;187:311-313. doi:10.1093/milmed/usac198
- Powers JG, Patel NA, Powers EM, Mayer JE, Stricklin GP, Geller AC. Skin cancer risk factors and preventative behaviors among United States military veterans deployed to Iraq and Afghanistan. J Invest Dermatol. 2015;135(11):2871-2873. doi:10.1038/jid.2015.238