Reducing the stigma and encouraging mental health care in the military
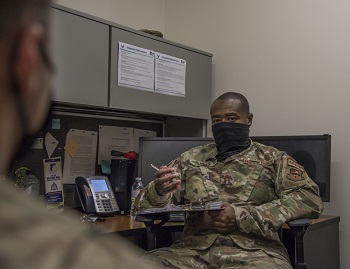
 Air Force Staff Sgt. Bradley Borytsky, a 28th Operational Medical Readiness Squadron alcohol and drug prevention and treatment technician (left), talks with Air Force Tech. Sgt. Andrew Collins, the 28th OMRS Mental Health flight chief, at Ellsworth Air Force Base, S.D., Oct. 7, 2020 (Photo by: Air Force Airman 1st Class Quentin K. Marx).
Air Force Staff Sgt. Bradley Borytsky, a 28th Operational Medical Readiness Squadron alcohol and drug prevention and treatment technician (left), talks with Air Force Tech. Sgt. Andrew Collins, the 28th OMRS Mental Health flight chief, at Ellsworth Air Force Base, S.D., Oct. 7, 2020 (Photo by: Air Force Airman 1st Class Quentin K. Marx).
In the military, the stigma of mental health is grounded in the cultural misperception that a service member must have "zero defects" to be mission ready.
While the Department of Defense strives to identify and eliminate barriers to care that service members face regarding mental health treatment, stigma remains a significant issue within the military.
Eliminating stigma starts with the individual, their immediate network (family, friends, and colleagues), and the broader community understanding that mental health is an element to overall health. Just as you would see your dentist to maintain oral health and a cardiologist to maintain heart health, seeking treatment for mental health concerns will help keep you in check to ensure you live a healthy, productive life.
Disseminating factual information about mental health care and engaging with service members to bust myths about mental health stigmas in the military can have the effect of encouraging someone who needs care to seek help.
Stigma around mental health care in the military may extend to career concerns, confidentiality, and perception of mental health care.
 Air Force Capt. Isaiah Jones (right), 59th Medical Wing licensed clinical social worker, speaks with a patient, Nov. 24, 2020, at the Mental Health Clinic, Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas. Mental health providers guide patients through challenging times, including stress or anxiety due to the pandemic, in person or through telehealth (Photo by: Air Force Airman 1st Class Melody Bordeaux).
Air Force Capt. Isaiah Jones (right), 59th Medical Wing licensed clinical social worker, speaks with a patient, Nov. 24, 2020, at the Mental Health Clinic, Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas. Mental health providers guide patients through challenging times, including stress or anxiety due to the pandemic, in person or through telehealth (Photo by: Air Force Airman 1st Class Melody Bordeaux).
"These are all barriers to care," said Marjorie Campbell, a clinical psychologist who leads the Psychological Health Center of Excellence's (PHCoE) Prevention and Early Intervention program.
"As a society, we place a premium on being able to take care of ourselves," she said. "In a nutshell, mental health is invisible, and people tend not to believe [in] things that they can't see."
Cultural and historical factors contribute to the belief that mental health disorders are in your head because you can't see them in the way you would a broken limb or a bleeding wound, so acknowledging them must mean you're weak, she explained. But this notion doesn't consider the physical symptoms of mental health on the brain.
She explained our thoughts are physical occurrences that result from the release of electrical and chemical activity. There are physiological underpinnings to every mental health disorder we experience, she said.
"Everything is interconnected," Campbell said. "You can't just separate out mental health and not consider that it's part of the organism."
Campbell, who has studied mental health stigma over time, noted the No. 1 reason service members give for not wanting to seek mental health care is they think they can handle problems on their own.
"That reveals preconceived stereotypes of self-reliance: 'I can do it,' 'I should be able to do it because I'm tough'," she said.
Another issue is treatment dropout, she said. An individual may start treatment because their spouse or their leadership may be pushing them, but they later drop out because they feel they can handle problems on their own. In the studies she saw, 63% of the people who dropped out said it was because they felt they could handle their problems on their own.
To reduce stigma, there are different levels at which an individual's community can intervene.
"As a provider, it's important to address an individual's concerns with stigma at the onset of treatment," she said. "If nothing is on the table, you can't deal with it."
She recommends providers be proactive and ask their patients how they feel about being there, if they are concerned about what other service members think or what their leaders think, and if they think it makes them feel weak.
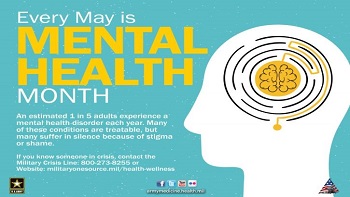 For Mental Health Awareness Month, Army Medicine wants to encourage those to help break the stigma associated with mental health disorders by supporting a friend, family member, or co-worker in need. Inspire them to seek treatment by providing an ear and the resources to get assistance (Photo by: Rebecca Westfall).
For Mental Health Awareness Month, Army Medicine wants to encourage those to help break the stigma associated with mental health disorders by supporting a friend, family member, or co-worker in need. Inspire them to seek treatment by providing an ear and the resources to get assistance (Photo by: Rebecca Westfall).
Separating the individual from the diagnosis clarifies that the diagnosis is a medical disorder, not one of choice or will.
To reduce stigma and reach those people reluctant to seek care requires a multi-pronged approach, "from the individual provider to Michael Phelps doing a commercial on TV for mental health to the policy work to the leader getting trained on how to support mental health, to the DOD's Real Warriors public awareness campaign," said Campbell.
It also takes ensuring service members know the facts around mental health. "They worry they won't be able to deploy, or will get separated out of the military, or that their unit leaders will find out about their diagnosis and perceive them as weak and make fun of them," said Campbell. "And, although sometimes those things happen, in general, we found that service members' perceptions of these barriers are not accurate."
She said that presenting the facts to them helps them realize mental health is not a deal breaker. "They might have heard one person say something, but this is not a career ender, even if sometimes some service members get medically discharged if they're not fit for duty."
PHCoE has more information on the barriers to care service members face regarding mental health diagnoses and treatment. It offers some do's and don'ts to consider when talking about mental health as well as some statistics on the barriers to mental health care impacting service members.