Background
The Centers for Disease Control and Prevention (CDC) defines Public Health Surveillance as "the ongoing, systematic collection, analysis, and interpretation of health data, essential to the planning, implementation, and evaluation of public health practice, closely integrated with the dissemination of these data to those who need to know and linked to prevention and control."1 Department of Defense (DOD) Directive 6490.02 defines comprehensive military health surveillance as "Health surveillance conducted throughout Service members' military careers and DOD civilian employees' employment, across all duty locations, and encompassing risk, intervention, and outcome data."2 While military health surveillance largely mirrors civilian practices, there are 2 main differentiating characteristics of military health surveillance. First, the military applies surveillance towards force health protection (FHP) and medical readiness to ensure a healthy and effective fighting force. The focus on the ability to work imparts military health surveillance with an occupational medicine component not seen in general civilian public health surveillance efforts. Second, surveillance occupies a central role in communicating health threats to military commanders to ensure both the health of the command and mission capability. Also, under military law the commander has intervention authorities not available in the civilian world. Other challenges differentiate military health surveillance from its civilian counterpart: its dynamic population, with continuous changes in membership; the mobility and geographic dispersion of the force; unique exposures possible during military service; and the public and political dimensions which can complicate the assessment of the effects of interventions.3
When the Defense Health Agency (DHA) was established, it had a mandate to consolidate the public health surveillance activities among the military services,4 which prompted a review of these capabilities. That review generated a report stressing the importance of surveillance to "enhance DOD's operational capabilities" and ensure a "ready, healthy, and fit" force to support Combatant Command objectives.5 This report also identified key weaknesses in surveillance at that time, including inaccessibility of data, fragmentation of processes and systems, poorly standardized and inconsistent practices, and lack of accuracy and relevance for current military operations.
To identify successes and failures that may inform how to best meet future needs, this historical review critically examines how Military Health Surveillance reporting systems have evolved over time. While the understanding of diseases, diseases of military importance, surveillance methods, and persons responsible for surveillance have changed over time, it is surveillance reporting as a tool to maintain operational readiness that has determined its impact and thus its importance in military activities.
Historical Origins of Military Public Health Surveillance (1662–1861)
Modern public health surveillance is often traced to the works of John Graunt in the 17th century, when he wrote the Observations on the Bills of Mortality of the city of London.6 Scholars remain divided on whether the Bills of Mortality were designed to keep track of the ability to field the militia in the face of public unrest, or to help monitor the need for public support of hospitals after the Reformation-based changes in church support of hospital charity. The data collected served both functions at different times, so the 2 areas of surveillance may have a common origin.
In the 1760s, the discipline of Military Medicine, in the sense of medical advice to ensure a healthy and mission-capable fighting force, began to establish itself in England. John Pringle's Observations on the Diseases of the Army and James Lind's An Essay on the Most Effectual Means of Preserving the Health of Seamen in the Royal Navy described the importance of monitoring the health of soldiers and sailors.7,8 Pringle counseled that "Tracing the more evident causes of military distempers, in order that whatever depended upon officers in command, and was consistent with the service, might be clearly stated, so as to suggest measures, either for preventing, or for lessening such causes in any future war."7
In the U.S., the military also began to collect health surveillance data for the purpose of preventive intervention before the civilian community. Prominent military physicians including Surgeon General (SG) James Tilton and Dr. James Mann recognized the importance of surveillance during the War of 1812 in order to control "camp diseases."9,10 These diseases fell into several categories including 1) childhood diseases such as smallpox and measles; 2) diseases of poor sanitation such as dysentery, diarrhea, and typhus; 3) geographic diseases such as malaria and yellow fever; 4) "inflammatory fevers" such as influenza and pneumonia; and 5) diseases associated with "Army life" such as trauma, sexually transmitted infections, and alcoholism.11 Dr. Mann recognized that these preventable sources of disease were "frequent causes of the failure of important expeditions, and ruin of armies; by which, the highest expectations of a nation are disappointed."10
Under SG Tilton, medical officers were first directed in 1814 to "make quarterly reports…of the sick and wounded… and report to the commanding officer every circumstance tending to restore or preserve the health of the soldiers."12 The problem he encountered was that these sick reports were only transmitted at the local level from the medical officer to the commander, and frequently, neither made any attempt to investigate the causes of illness or prevent their further occurrence. Furthermore, reporting was not standardized. Many surgeons provided little or no information, while others offered detailed data and narrative accounts of the impact of diseases on their forces. Finally, the imprecisely defined nature of the conditions, and the use of counts rather than rates, frequently impaired meaningful interpretation or public health use. There were several reasons for this imprecision, the most important of which was likely that the traditional purpose of reporting was to determine the number of trained soldiers ready to fight. Another important issue was that the understanding of the relationships between the multiple proximal and distal causes of most diseases were often not clear or not amenable to modification in military life. These problems persisted, even when the War Department issued regulations in December 1814, which directed medical officers to keep records of this comprehensive system of monthly and quarterly reports, including "the appearance of epidemics."13 Because of these problems, the corresponding impact of surveillance on military readiness was relegated to the local level at which surveillance was conducted.14
As detailed in a recent book by Colonel (Ret.) Steve Craig, the power of health surveillance as a guide for disease prevention was not realized until 1818, when the Army appointed Joseph Lovell as the first permanent SG and established the Army Medical Department.15 Before his appointment, SG Lovell's 1817 report to the Commanding Officer of the Northern Division on the causes of disease in the Army stressed that "every surgeon… should consolidate the quarterly reports; and make such remarks and suggest such improvements both in practice and police, as may appear to be required for the benefit and comfort of the sick… And finally from his own observations, and from the reports and accompanying remarks of the surgeons, to form a manual of medical police and practice suited to the circumstances of the soldier; and to make such reports to the commanding general..."16
Upon his appointment as Surgeon General in 1818, SG Lovell instituted immediate changes through the Regulations of the Medical Department. These regulations required a standardized format that the surgeons (i.e., any physician) "make quarterly reports of sick to the Surgeon General, and morning reports to the commanding officer, in the form and manner directed for the surgeons of the army," in order to "discover as far as practicable the probable causes of disease, and recommend the best means of preventing them."17 The SG would further "receive such reports and returns from [the surgeons]," which, in turn, would enable him to communicate to the Secretary of War "such remarks relative to improvements in practice and police… as may seem to be required for the preservation of health." These regulations sought to ensure that health data were communicated to the SG rather than just to the command, and to create a "medical police" to enforce the prevention of disease. "Police" during this period meant policy and procedure rather than personnel, but it was still an effort to improve health conditions in a systematic way.
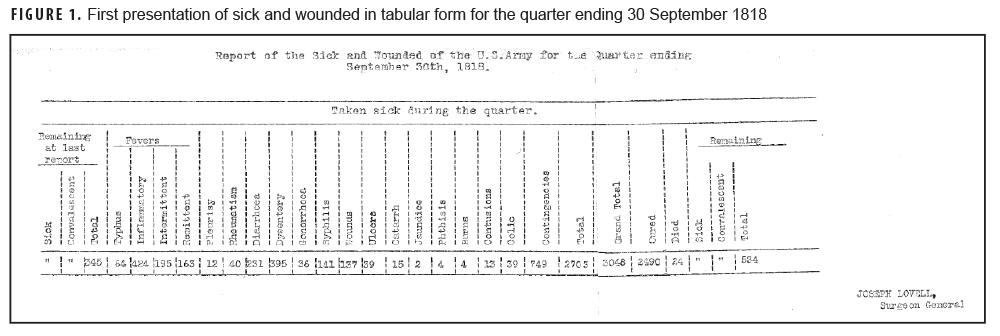
In the first of the SG's reports, SG Lovell concluded that the Commanders who followed his rules for medical police had regiments that are "worth at least three of those whose soldiers [did not follow these rules]…"18 The most important diseases in these early reports again emphasized the "camp diseases" of military importance, as seen in the first tabular display of these data from 1 Sept. 1818 (Figure 1). Although the exact pathologies of these diseases were not known at the time, they were heavily influenced by environmental and sanitary conditions that could be modified by Lovell's "medical police." By submitting these quarterly reports to the Secretary of War, SG Lovell used health data to advocate for conditions that would prevent common diseases and promote the health of the Army—such as improvements in environmental conditions, better food and clothing, and "abolition of the whiskey ration."16 SG Lovell also began submitting a published, annual report to the Secretary of War in 1822. Although the annual report at first was solely a financial accounting of the medical department, it gradually introduced surveillance and sanitary data, including the first statistical table of morbidity in the 1835 report.17
In 1840, SG Lawson began compiling its quarterly reports into statistical surveillance reports using new techniques of rates and stratification developed by the British epidemiologist William Farr.19 In addition to the data on illnesses and climatic/ environmental data from the surgeons' reports, these reports included the use of population-based denominators obtained from non-medical sources, i.e., the Adjutant General. These reports again emphasized the need to use this information for public health practice, now called "military hygiene," that was defined as "the knowledge of maintaining the health of soldiers, and of promoting their efficiency." It was not until 1850 that similar work incorporating statistical analysis of health data to inform public health practice was begun outside of military populations in Massachusetts by Lemuel Shattuck.20 The success of SG Lawson's efforts at improving sanitation and the health of the Army through these reports is evident in the documented improvements in health demonstrated in subsequent surveillance reports, such as the use of vaccination to reduce smallpox transmission or quinine to control malaria.21 A notable exception was during the Mexican-American War between 1846 and 1848, during which no comprehensive reports other than mortality were available due to the difficulties of transmitting these reports across the frontier.22, 23 In 1842, the Bureau of Medicine (BUMED) also began reporting to the Secretary of Navy, but these reports initially consisted of only financial accounts rather than reports of important diseases.24 By 1860, however, BUMED was compiling sick reports and performing analyses similar to Army reports.25
Expansion and Institutionalization of Military Public Health Surveillance (1861–1945)
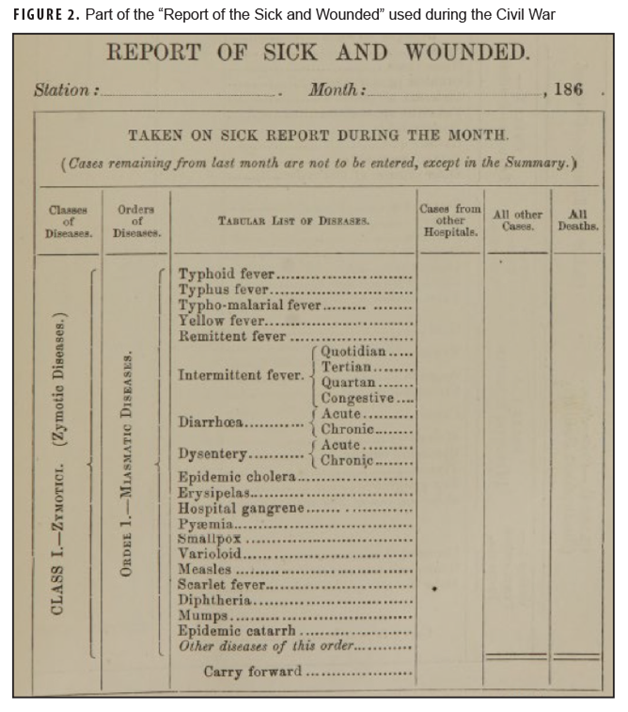
Up to the beginning of the Civil War, the quarterly reports by surgeons continued as before, while additional, more rigorous statistical analyses of these reports were compiled in 185623 and 1860.21 There was a broad, emerging appreciation of the medical hazards of mobilization based on the reported Crimean War experience of the British as revealed by the work of Florence Nightingale.26 After the first year of the Civil War, however, the "Sick and Wounded" reports were found to be "insufficient and defective," leading SG William Hammond to order "more detailed and exact reports" from his medical officers.27 In 1863, General Order Number 355 was promulgated in Circular Number 25, stating that "all obtainable statistics and data" should be compiled and forwarded to the SG, with particular attention paid to sanitation, medical supplies, environmental factors, the nature of the injuries, and other epidemiologic information. An example of a part of 1 of these reports "miasmatic diseases" is shown in Figure 2. The understanding of disease pathology was limited at the time, but the classification of disease in these reports was consistent with those published by Dr. Farr, including these major groups: zymotic (contagious), constitutional (e.g., tuberculosis), parasitic, local (e.g., eyes, ears), and wounds/injuries.27,28 SG Hammond also directed his Medical Officers to "diligently collect and preserve…pathological surgical specimens."28 Although this was originally intended to better understand the treatment of battle injuries, this collection and study of pathological specimens also enabled a better understanding of "camp diseases" such as typhoid and malaria.
These experiences also had a profound impact on the large number of American physicians in the Union Army and shaped an appreciation of medical sciences and public health after the war.29 The information from these reports was published after the war in a multi-volume set, The Medical and Surgical History of the War of Rebellion, which greatly expanded the scope of the previous (peacetime) Reports of the Surgeon General in size, scope, complexity, and detail.27 Professor Rudolph Virchow, the father of modern pathology and founder of social medicine, was "astounded by the richness" of these reports, praising them for "the utmost accuracy of detail, the painstaking statistics embracing the minutest details…comprehending every aspect of the practice of medicine…in order to preserve and transmit to contemporaries and posterity, in the most thorough way possible, the wisdom purchased at so great a price."30 These developments demonstrate the increased importance of surveillance data to support wartime operations compared to peacetime, as well as the influence military health surveillance on civilian public health practice. However, none of these reports were published during the Civil War itself, as the SG's office did not have the resources to publish the massive quantities of data in a timely fashion.30 In 1872, military medical officers, members of the new Marine Hospital Commissioned Corps (later the Public Health Service), and urban practitioners responsible for public health gathered in Atlantic City to form the American Public Health Association, beginning a process of professionalization and standardization in public health examinations and reporting. Their work would be synergistic with Army efforts for several generations.
Within a few years after the end of the Civil War, the Reports of the Sick and Wounded returned to their prewar size, averaging less than 10 pages in the late 1860s and 14 pages in the 1870s, and the reports contained no detailed information on specific diseases of military importance. This reduction in the length and level of detail of the report suggests the trend of military leaders recognizing the relevance of surveillance during times of conflict but less so after the cessation of conflict.
Nevertheless, the example of the Medical and Surgical History inspired young Americans to study the new sciences in Europe, and the methods of military and civilian public health surveillance evolved dramatically with advances in science and medicine over the next several decades. These advances included the understanding of the etiology of diseases (e.g., germ theory and laboratory diagnosis), statistical techniques such as rates and stratification, and specialization of surveillance activities.
Dr. George Sternberg brought many of these advances to military use through his pioneering personal use of microscopy to study bacteria and disinfection.31,32 Upon being named SG in 1893, he immediately established the Army Medical School to increase the military's preparedness through military medical education, with an emphasis on sanitation and laboratory diagnosis.33 William Osler, who is considered by many the father of modern medicine, would later describe the Army Medical School as America's first school of public health.34 The military also developed innovative epidemiologic approaches relevant to military readiness. For example, the Army and Navy SG's surveillance reports were the first to track disability outcomes such as lost duty time and medical discharges, which was not standard practice in civilian occupational health surveillance until the early 20th century.35 By 1883, the Army report had increased in size to 43 pages, and by the 1890s each volume averaged 150 pages.
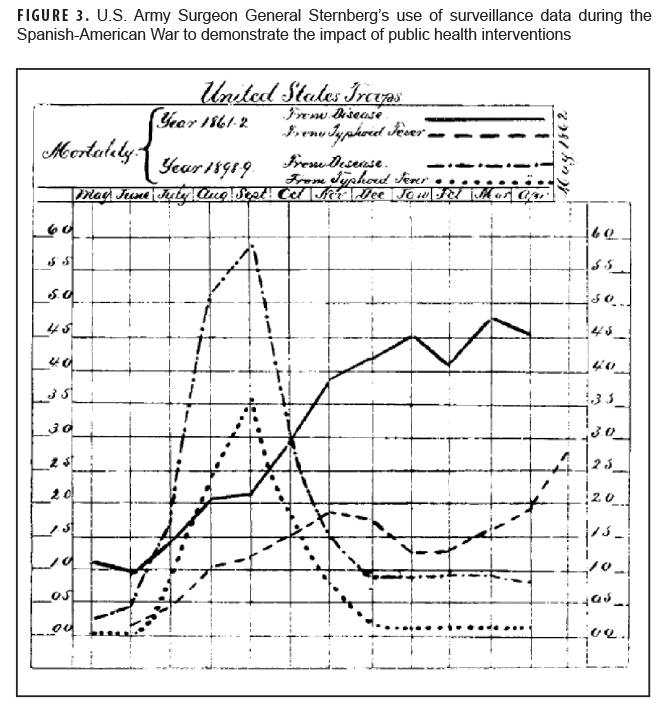
The scope, complexity, and detail of the SG's surveillance reports further expanded during the Spanish-American War due to the impact of health threats encountered in tropical locations, such as malaria, typhoid, and yellow fever. SG Sternberg credited the reductions in mortality and improvements in the health of the Army, that were demonstrated in surveillance reports during the War, to "energetic measures" in sanitation and hygiene.36,37 An example of this is illustrated in Figure 3, which demonstrates the impact of prevention efforts on mortality from typhoid and compares the Army's experience with typhoid fever during the Spanish-American War with that of the Civil War. The impact of military public health surveillance was further realized in detailed, in-depth outbreak and epidemiologic investigations such as the Typhoid Fever Board. SG Sternberg originally appointed Major Walter Reed to investigate and control an epidemic of undiagnosed febrile disease that was causing morbidity and mortality in U.S. military camps. The resulting application of surveillance and epidemiologic investigation of this typhoid outbreak led to the initiation of water sterilization and other improvements in sanitation and hygiene and dramatic declines in morbidity and mortality.38
The recognition of the power of timely data, captured by Sternberg in his publication of the lessons of the war with Spain, also impacted the British in their deployments to South Africa and the Japanese in their 1905 war with Russia.36,37 Well-trained military medical officers with both adequate laboratory support, as well as access to Commanders who could order the change in field conditions, had the ability to save lives and significantly preserve the unit's fighting strength. Following the Spanish-American War, the basic reporting of monthly health surveillance data was performed in the Army through Form 51, which continued to be called the "Report of Sick and Wounded."39 In 1914, the Chief Surgeon during the U.S. occupation of Veracruz recognized the need for weekly and even daily reporting of casualties and communicable diseases and directed more prompt reporting of the health status of the Army.22 This report was adopted for use in other settings, including by the American Expeditionary Forces (AEF) during World War I. Of note, the SG's office encountered difficulties in estimating strength (denominator) data due to inconsistencies between the numbers in the medical reports and the reports to the Adjutant General's office, as well as delays in getting accurate data due to the "necessity for secrecy."39
After World War I, surveillance reports were published with a scope, complexity, and detail never before seen in the U.S. Military, again suggesting their importance and impact in assessing FHP and readiness.39 These reports showed increasingly sophisticated graphical displays of data and incorporated medical advances such as new laboratory and radiography diagnostics used to mitigate tuberculosis (TB) and typhoid.40–42 The impact of these surveillance reports on FHP and readiness was demonstrated by the low rates of TB and typhoid transmission among U.S. forces compared to the other major combatants.40,42 Surveillance for chronic health, behavioral health, and other non-communicable diseases was also increasingly conducted due to its potential impact on military readiness and operations.41 After World War I, surveillance in the Report of the Surgeon General again began to decline in size, scope, complexity, and detail. With the advent of World War II, once again a flurry of surveillance activity occurred. Reports became more detailed and encompassed an increasingly broad scope of the military's worldwide operations, although again much of the surveillance data would not be accessible in published reports until after the end of the war. A board was established to study the feared impact of respiratory diseases in barracks, and it became the first of a series of commissions on various classes of infections that impacted mobilization.43 As in World War I, civilian experts from academic medical centers were brought into these commissions to supplement undermanned military staffs. These commissions were collectively called the Army Epidemiological Board, later renamed the Armed Forces Epidemiological Board (AFEB) after the war (it is now called the Defense Health Board). The AFEB addressed FHP threats such as acute respiratory diseases, influenza, enteric infections, vaccinations, and others.44 The goal of these commissions was similar: to reduce the impact of these diseases on military readiness. Surveillance activities were therefore a critical component of ensuring readiness by monitoring the burden of disease, trends, and effectiveness of interventions aimed at their control.
The impact of the military's varied and enhanced prevention efforts, including surveillance, on FHP and readiness was demonstrated by World War II being the first conflict during which the number of fatalities caused by disease was less than those caused by battle.45 Specific examples showing the impact of surveillance data include demonstrating that the vast majority of TB cases existed prior to military service,46,47 documenting the effectiveness of malaria control efforts in endemic areas,48 and in communicating to commanders the importance of sanitation efforts in preventing diarrhea and dysentery.49
Modern Military Health Surveillance (1945–present)
The modern concept of public health surveillance was formalized after World War II by Alexander Langmuir at the Communicable Disease Center, the precursor of the modern CDC.50 While surveillance activities had been taking place previously in military and civilian settings, this was the first real use of the term "surveillance"—previously these activities were called "reports" or "statistics." Nevertheless, the name Langmuir chose was significant in making explicit the importance of the systematic nature of the collection and evaluation of health data, as well as the need for communication to stakeholders and policy development. Langmuir further built the Epidemic Intelligence Service (EIS), with its central training of local experts, to assure systematic and consistent standards in public health surveillance and disease outbreak investigations, particularly for biothreat agents.51
After World War II, the services pulled their public health surveillance portions out of the Report of the Surgeon General and made them into monthly publications called The Health of the Army and Statistics of Navy Medicine (Figures 4a, 4b). In contrast to the periods after previous conflicts, these reports were not reduced in scope, complexity, and detail. Instead, these reports provided detailed, up-to-date articles on topics of military and public health significance which impacted military operations and readiness. The Navy determined that the Annual Report of the Surgeon General could not meet the "planning needs of an active medical department either changes that need to be made in such policies."53 The continued importance of surveillance seen even after the conclusion of the war is probably due to the continued operations in both the European and Pacific Theaters despite the end of hostilities, as well as the close proximity in time to the onset of the Korean War. For the first time after the end of a military conflict, the U.S. did not drastically reduce its armed forces, but rather kept a frequently drafted, worldwide based, standing military force that was forward-deployed in support of the Cold War. Although communicable diseases continued to occupy a prominent place in these Cold War-era reports, increasing attention was paid to issues of non-effectiveness, hospitalization, medical evacuation, mortality, and civil public health. Despite their quality and utility, few of these reports are accessible today because they were published as "gray" literature, meaning that they are not commonly available in medical libraries, nor are they found in PubMed or other similar databases.
With improvements in medical care, access, and overall health status in the U.S. population, outpatient care assumed a growing importance in assessing the burden of disease in surveillance data.20 Both outpatient and inpatient reports continued to occupy a prominent place during the Vietnam War, during which surveillance continued to impact military operations and readiness. For example, malaria rates were shown to be associated with geography, climate, enemy contact, preventive measures, and command discipline.54
During this time, military authors increasingly communicated their public health surveillance data in the peer reviewed medical literature rather than in internal military documents and publications. The greater accessibility and recognition of these journals by the non-military medical community made them more attractive vehicles for authors to publish military surveillance data. However, this led to fragmentation of the literature and sometimes mixed messages. An example of this is the differing reports regarding the risk of TB disease and skin test conversion resulting from deployment to Vietnam, which led to conflicting assessments about the effectiveness of control measures and need for additional control measures.55–61 It also led to the demise of the Health of the Army and Statistics of Navy Medicine, which began to decrease in complexity, detail, and scope, with a corresponding decrease in their relevance and impact. By the mid-1980s these reports contained only large quantities of computer-generated tables of health care utilization data without any analysis or relevance to improving FHP or readiness. Ultimately, the publication of both reports ended by 1988.
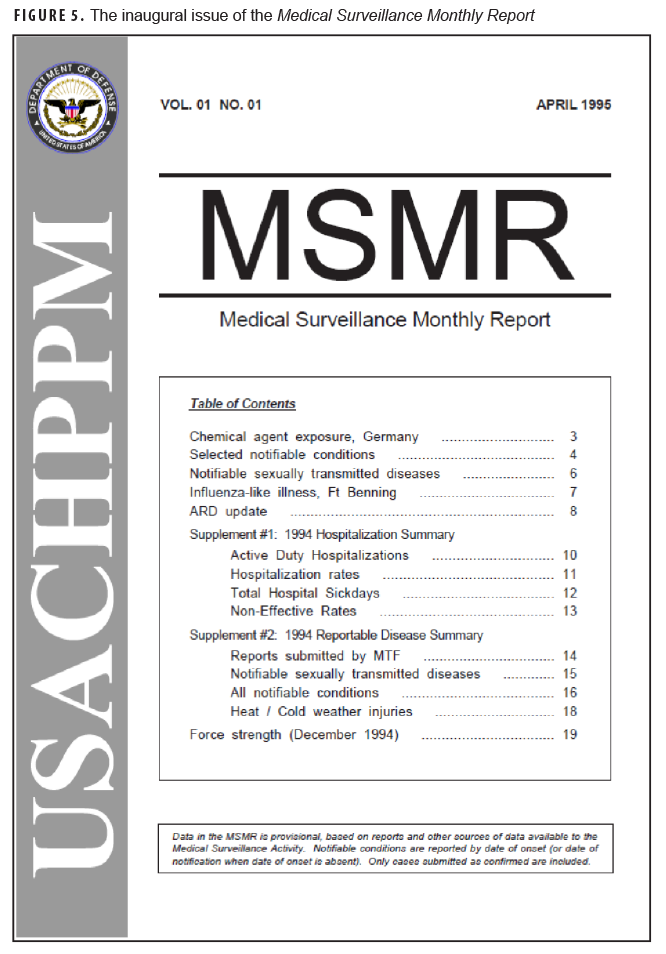
In 1995, the Army Medical Surveillance Activity (AMSA) began publishing the Medical Surveillance Monthly Report (MSMR) (Figure 5). The purpose of the MSMR was "to provide readily available information necessary to inform, motivate, and empower commanders, their surgeons, and medical staffs to design, implement, and resource programs that enhance health, fitness, and readiness."62 This publication, patterned on the CDC's Morbidity and Mortality Weekly Report, marked the first real use of the terms "surveillance" and "readiness" in military public health reports. Major strengths of the MSMR included 1) its access to all administrative health data through the Defense Medical Surveillance System (DMSS);3 2) its accessibility to military and civilian health professionals, as it had free full text from its inception and was first indexed in Medline in 2011; and 3) its scientific credibility through its peer review process and editorial independence.63 Initial reports were similar to the Health of the Army reports, with tabular data, analysis, and recommendations for public health action. While current reports still have this format, they often use modern statistical methods such as regression and advanced laboratory methods such as genotyping or other molecular testing. The focus of the surveillance has also changed. In 1995, 66% (59/90) of articles were on communicable disease topics such as HIV infection and other sexually transmitted infections, adenovirus and other respiratory infections, and malaria and other vector-borne infections. By 2020, this proportion had dropped to 40% (20/50), with the other topics including public health issues such as heat and cold weather injuries, medical evacuations, cardiovascular diseases, opioid use, and mental health disorders.
In 2015, the Army began publication of a surveillance report called The Health of the Force, the goal of which was to "track the health of the Army…to improve the health readiness of the Total Force."64 This report focused almost entirely on non-communicable health factors, including lifestyle factors such as physical activity, obesity, and tobacco use, behavioral health conditions, occupational and environmental exposures, injuries, and other factors affecting military medical readiness. This report not only provided surveillance data at a force-wide and local installation level, but also examined interventions aimed at promoting health, how they were implemented, and their impact on health and readiness at different installations. However, because the report was published as gray literature it had limited accessibility, credibility, and overall impact. The Army, Navy, and Air Force public health hubs all routinely publish other surveillance data in both the gray literature and in the scientific literature.
How can history inform current and future military health surveillance?
While the understanding of diseases of military importance, laboratory and statistical surveillance methods, and persons responsible for this surveillance have evolved over time, it is the linkage towards maintaining readiness that has determined the impact and thus the success of military public health surveillance. Surveillance has gone from an activity practiced primarily by general medical officers to an activity primarily led by specialists in preventive medicine and public health. Furthermore, although the miasmatic understanding of disease has evolved to germ theory and the molecular basis of disease, the underlying principles and purpose of public health surveillance in the military have remained consistent: ensuring the readiness of the fighting force in times of both peace and in conflict.
Although military health surveillance has developed remarkably over the past 200 years, several limitations remain. The DHA's recent capabilities-based assessment found shortfalls in the areas of accessibility of data, integration of processes and systems, standardization of practices of key findings efficiently and effectively to commanders, and evaluation.5 Surveillance data are not useful if the information is considered invalid or do not address public health issues in a timely fashion. An important challenge for public health surveillance is the potential for misclassification of exposure, as demonstrated by the challenges in quantifying exposures to Agent Orange in the Vietnam War or burn pits in the Iraq and Afghanistan conflicts.65,66 Military health surveillance must ensure that it encompasses rigorous, up-to-date laboratory and statistical methods in order to maintain credibility within both military and civilian medical and public health communities. For these reasons, peer-reviewed, scientifically-credible reports such as those found in the MSMR are powerful tools that promote impact through accessibility and strategic communication, and these should be promoted and expanded. This review does not consider formal or informal surveillance activities which may be extremely important but for which no accessible documentation or reports exist. These include public health surveillance information provided to inform Commanders of health threats in real time, or actionable surveillance provided by the Armed Forces Health Surveillance Division's Electronic Surveillance System for the Early Notification of Community-Based Epidemics (ESSENCE) or Health Surveillance Explorer (HSE) available at https://health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Branch.
Public health has achieved its greatest impact during times of conflict, when prevention and medical readiness are directly tied to the success of the operational mission. When the impact of medical readiness and prevention activities are not considered as important, surveillance activities are correspondingly undervalued. The case for maintaining a robust military public health surveillance capability is therefore closely aligned with the case for maintaining prevention activities in support of FHP and readiness. As stated by Brigadier General Love more than 50 years ago, the effectiveness of surveillance activities "depends in large part upon its responsiveness to current problems and developing trends in military and medical affairs."22 Public health personnel must maintain a linkage to medical and public health policy makers, in particular non-medical military leaders, to ensure that the most important public health issues are identified, communicated, and acted upon. Finally, as the CDC was integral in federalization of state and local public health departments, so too can a central body such as the DHA standardize joint service data collection and reporting so that it can be better aggregated centrally and more easily accessed to inform policy and improve health. These are the historical lessons of military public health surveillance that must be considered as DHA develops the military's public health surveillance system of the future.
Author affiliations: Department of Preventive Medicine & Biostatistics, Uniformed Services University of the Health Sciences (USUHS), Bethesda, MD (COL Mancuso and CPT Pierson); Division of Medicine, U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID), Fort Detrick, MD (CPT Pierson); Departments of Preventative Medicine & Biostatistics and Military & Emergency Medicine, Uniformed Services University of the Health Sciences (USUHS), Bethesda, MD (Dr. Smith).
References
- Hall HI, Correa A, Yoon PW, Braden CR; Centers for Disease Control and Prevention. Lexicon, definitions, and conceptual framework for public health surveillance. MMWR Suppl. 2012;61(3):10–14.
- Under Secretary of Defense for Personnel and Readiness (USD[P&R]). DoD Directive 6490.02E: Comprehensive Health Surveillance (Change 2, 28 August 2017). In: Department of Defense, ed2012.
- Rubertone MV, Brundage JF. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002;92(12):1900–1904.
- 115th U.S. Congress. John S. McCain National Defense Authorization Act for Fiscal Year 2019. Accessed 28 Jan 2019. https://www.congress.gov/bill/115th-congress/house-bill/5515/text#tocHD897E49C86064423BDD0D0B62327A58A
- Office of the Assistant Secretary of Defense (OASD) for Health Affairs (HA), Public Health Division of the Defense Health Agency (DHA). Comprehensive Health Surveillance (CHS) Capabilities-Based Assessment (CBA) Study Report. In: Department of Defense, ed. Falls Church, VA; 2017.
- Graunt J. Observations on the Bills of Mortality 1662. Accessed 7 March 2021. http://www.edstephan.org/Graunt/bills.html
- Pringle J. Observations on the diseases of the army (1st American Edition). Philadelphia, PA: Edward Earle; 1810.
- Lind J. An essay on the most effectual means of preserving the health of seamen, in the Royal Navy. London: Printed for D. Wilson; 1762.
- Tilton J. Economical Observations on Military Hospitals; and the Prevention and Cure of Diseases Incident to an Army. Wilmington, DE: J. Wilson; 1813.
- Mann J. Medical Sketches of the Campaigns of 1812,13,14. Dedham, NH: H. Mann and Co.; 1816.
- Barboriak PN. Reporting to the Surgeon General: The peacetime practice of military surgeons in antebellum America, 1818-1861. Ann Arbor, MI, Duke University; 1987.
- Palmer TH, ed The Historical Register of the United States. Part I. For 1814. Vol. III. Philadelphia, PA: G. Palmer; 1814.
- War Office. Regulations for the Medical Department. In: Brown HE, ed. The Medical Department of the United States Army from 1775 to 1873. Washington, DC: Surgeon General's Office; 1814.
- Brown HE. The Medical Department of the United States Army from 1775 to 1873. Washington, DC: Surgeon General's Office; 1873.
- Craig SC. "Some System of the Nature Here Proposed". Fort Sam Houston, TX: Office of the Surgeon General: Borden Institute; 2015.
- Lovell J. Remarks on the Sick Report of the Northern Division for the Year Ending June 30th 1817. In: Craig SC, ed. "Some System of the Nature Here Proposed". Fort Sam Houston, TX: Office of the Surgeon General: Borden Institute; 1817.
- The Army Surgeon General. Regulations of the Medical Department, Sept. 1818. In: Brown HE, ed. The Medical Department of the United States Army from 1775 to 1873. Washington, DC: Surgeon General's Office; 1818.
- Lovell J. Report of the Surgeon General: Surgeon General's Office, Nov. 1st, 1818. In. Washington, DC: Surgeon General's Office; 1818.
- Forry S. Statistical report on the sickness and mortality in the Army of the United States. Washington, DC: Jacob Gideon, Jr.; 1840.
- Shattuck L. Report of the Massachusetts Sanitary Commission. Cambridge, MA: Harvard University Press; 1850.
- Coolidge RH. Statistical report on the sickness and mortality in the Army of the United States; embracing a period of five years, from Jan. 1855, to Jan. 1860. Washington, DC: George W. Bowman; 1860.
- Love AG, Hamilton EL, Hellman IL. Tabulating Equipment and Army Medical Statistics. Washington, DC: Office of the Surgeon General; 1958.
- Coolidge RH. Statistical report on the sickness and mortality in the Army of the United States; embracing a period of sixteen years, from January, 1839, to January, 1855. Washington, DC: A.O.P. Nicholson; 1856.
- Department of the Navy. Annual Report of the Secretary of the Navy. 1842. Accessed 18 Feb 2019. https://www.history.navy.mil/content/dam/nhhc/research/library/online-reading-room/history-of-the-us-navy/secnavreports/1842-annualreportsecnav-adddocs.pdf
- Department of the Navy. Annual Reports of the Navy Department: Report of the Secretary of the Navy. 1861. Accessed 18 Feb 2019. https://babel.hathitrust.org/cgi/pt?id=osu.32435052548781;view=1up;seq=11
- British National Archives. Report on medical care. Accessed 7 March 2021. https://www.nationalarchives.gov.uk/battles/crimea/popup/medical.htm
- U.S. Surgeon General's Office. The Medical and Surgical History of the War of the Rebellion, 1861-1865. Washington, DC: Government Printing Office; 1870.
- Woodward JJ. Outlines of the Chief Camp Diseases of the United States Armies As Observed During the Present War. Philadelphia, PA: J.B. Lippincott & Co; 1863.
- Devine S. Learning from the Wounded: The Civil War and the Rise of American Medical Science. Chapel Hill, NC: UNC Press; 2014.
- Love AG. Some of the History of the Annual Report of the Surgeon General, with Extracts. Chicago, IL: Blakely-Oswald Printing Company; 1913.
- Sternberg GM. Malaria and Malarial Diseases. New York: William Wood & Company; 1884.
- Sternberg GM. A Manual of Bacteriology. New York: William Wood & Company; 1893.
- Craig SC. In the Interest of Truth: The Life and Science of Surgeon General George Miller Sternberg. Fort Sam Houston, TX: Borden Institute; 2013.
- Osler W. The Army Surgeon. The Medical News. 1894;64:1–12.
- Institute of Medicine Committee to Assess Training Needs for Occupational Safety and Health Personnel in the United States. Safe Work in the 21st Century: Education and Training Needs for the Next Decade's Occupational Safety and Health Personnel. Washington, DC: National Academies Press; 2000.
- Sternberg GM. The Work of the Army Medical Department During the Spanish War. JAMA. 1898;31:1356–1360.
- 37. Sternberg GM. Sanitary Lessons of the War. JAMA. 1899;32(23):1287–1294.
- Reed W, Vaughan VC, Shakespeare EO. Report on the Origin and Spread of Typhoid Fever in U.S. Military Camps during the Spanish War of 1898 Washington, DC: Government Printing Office; 1904.
- Love AG. The Medical Department of the United States Army in the World War, Volume XV: Part 2, Medical and Casualty Statistics. Washington, DC: Government Printing Office; 1925.
- Bushnell G. Tuberculosis. The Medical Department of the United States Army in the World War (The Official History Series) Communicable and Other Diseases, Volume IX. Washington, DC: Government Printing Office; 1928.
- Office of the Surgeon General. Reports of the Army Surgeon General to the Secretary of War, 1918–1920. Washington, DC: Office of the Surgeon General; 1918–1920.
- Siler J, Lambie J. Typhoid and the paratyphoid fevers. In: Lynch C, Weed F, McAfee L, eds. The Medical Department of the United States Army in the World War, Vol IX. Washington, DC: Office of the Surgeon General, Department of the Army; 1928.
- Jordan WS. Commission on Acute Respiratory Diseases Incorporating Three Other Commissions. In: Woodward TE, ed. The Armed Forces Epidemiological Board. The Histories of the Commissions. Washington, DC: Borden Institute; 1994.
- Woodward TE, ed. The Armed Forces Epidemiological Board. The Histories of the Commissions. Washington, DC: Borden Institute; 1994.
- Smallman-Raynor MR, Cliff AD. Impact of infectious diseases on war. Infect Dis Clin North Am. 2004;18(2):341–368.
- Long ER, Hamilton EL. A Review of Induction and Discharge Examinations for Tuberculosis in the Army. Am J Public Health Nations Health. 1947;37(4):412–420.
- Long ER. The tuberculosis experience of the United States Army in World War II. Am Rev Tuberc. 1947;55(1):28–37.
- Denit G. Message from the Chief Surgeon in the Far East. Bull US Army Med Dept. 1945;86:53.
- Philbrook F, Gordon J. Diarrhea and Dysentery. In: HOFF E, ed. Preventive Medicine in WWII, Volume IV, Communicable Diseases, Transmitted Chiefly Through Respiratory and Alimentary Tracts. Washington, DC: Office of the Surgeon General, Department of the Army; 1958.
- Langmuir AD. The surveillance of communicable diseases of national importance. N Engl J Med. 1963;268:182–192.
- Langmuir AD, Andrews JM. Biologcal Warfare Defense: The Epidemic Intelligence Service of the Communicable Disease Center. Am J Public Health. 1952;42:235–238.
- Bureau of Medicine and Surgery. The Launching Statistics of Navy Medicine. Sept. 1945;1(1).
- Office of the Surgeon General. Notes and Definitions. Health of the Army. 31 July 1946;1(1):55.
- Neel S. Medical support of the U.S. Army in Vietnam, 1965–1970. Washington, DC: Government Printing Office; 1973.
- Mancuso JD. Tuberculosis Screening and Control in the US Military in War and Peace. Am J Public Health. 2017;107(1):60–67.
- Sowell JM, Russell RM, Ionata VJ. Tuberculin tine test conversion among United States Army enlisted personnel in Vietnam. Mil Med. 1973;138(2):96–98.
- Sachs JM, Miller CH. Tuberculin skin-test conversion in Vietnam. 1969 annual skin-test reports of Navy and Marine Corps. Ann Intern Med. 1970;73(5):767–769.
- Cowley RG. Implications of the Vietnam war for tuberculosis in the United States. Arch Environ Health. 1970;21(4):479–480.
- Cowley RG, Briney RR. Primary drug-resistant tuberculosis in Vietnam veterans. Am Rev Respir Dis. 1970;101(5):703–705.
- Dantzker DR, Steinberg HN, Kmiecik JE. Primary drug-resistant tuberculosis in Vietnam veterans 1967 to 1970. Am Rev Respir Dis. 1972;106(2):273–274.
- Harris JO, Lischner MW. Tuberculosis in active duty military personnel. Mil Med. 1973;138(7):427–429.
- Brundage JF. The Medical Surveillance Monthly Report (MSMR): A Mirror on the Health, Fitness, and Medical Readiness of America's Army. Med Surv Monthly Report. 1995;1(1):2.
- Brundage JF, Rubertone MV. Medical Surveillance Monthly Report: The first 20 years. MSMR. 2015;22(4):2–4.
- Army Public Health Center. Health of the Force. Accessed 2 January 2021. https://api.army.mil/e2/c/downloads/419337.pdf
- Boyle CA, Brann EA. Proxy respondents and the validity of occupational and other exposure data. The Selected Cancers Cooperative Study Group. Am J Epidemiol. 1992;136(6):712–721.
- Garshick E, Abraham JH, Baird CP, Ciminera P, et al. Respiratory Health after Military Service in Southwest Asia and Afghanistan. An Official American Thoracic Society Workshop Report. Ann Am Thorac Soc. 2019;16(8):e1–e16.