Reducing preventable injury and illness enhances the readiness of the Armed Forces, as illnesses and injuries degrade service member readiness and can hinder mission accomplishment. Since 2012, the MSMR has used a classification system derived from the Global Burden of Disease Study,1,2 in combination with an International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) chapter-based system to broadly describe the morbidity burden among active component service members and categorize hospitalizations and ambulatory visits among this population. The MSMR editorial staff continues to refine these classification schemes to improve the usefulness of the information presented.
In these annual burden of disease reports, the MSMR groups diagnoses to inform our readership of the major drivers of health care utilization within the Military Health System and where changes in policy or preventive emphasis may improve the medical readiness of the force. The major classification system for diagnoses, ICD-10-CM, features over 68,000 separate codes, a more than 5-fold increase from the 13,000 codes available in the previous version (ICD-9-CM).2 While the ICD-10-CM is organized in logical chapters, the groupings are not optimized to describe burdens of disease in a military population. A delicate balance between “lumping” and “splitting” of diagnoses is required to achieve a meaningful portrayal of the burden in the military population.
The burden of disease in a young, healthy, predominantly male service member population will differ substantially from the general U.S. or global populations. The numerous readiness-related ambulatory visits required of each active duty service member, as well as military living circumstances, training requirements, and access to medical care without cost, may contribute to differing morbidity burden profiles in comparisons to other populations. Unique distributions in population demographics require, at a minimum, age and gender adjustment when comparing military rates to other populations. Typical adjustments are often insufficient to compensate for these unique factors, making comparisons challenging.
Demographic differences are particularly striking when comparing the active component to the general U.S. population. Service applicants are medically screened prior to military service to ensure fitness requirements for physically demanding jobs, and throughout their service mandatory periodic (typically annual) health assessments and screenings among active component members may detect conditions potentially undetected in other populations. People enlist or are commissioned into the active component, typically between 17 and 25 years of age, with the end of service for nearly all members by age 50. In 2022, the mean age of active component service members was approximately 29, with less than 1% of the population over 50.3 By contrast, the median age of the U.S. population was 38.7, with 36.1% over age 50 in 2021.4 Women constituted 17.5% of the active component in 2022, compared to 51.0% in the general U.S. population.4
Within the military population and its specific settings, categories of illnesses and injuries requiring hospitalization have historically differed from those resulting in the most ambulatory visits. The added requirements for readiness are likely a major factor in ambulatory health care utilization, but rarely for hospitalization. The categories of medical conditions and readiness requirements that account for the most medical encounters overall may differ from those that affect the most individuals or have the most debilitating or long-lasting effects.1
This annual summary uses several health care burden measures to quantify the impacts of various illnesses and injuries in 2022 among members of the active component of the U.S. Armed Forces. Health care burden metrics include the total number of medical encounters, individuals affected, and hospital bed days.
What are the new findings?
Provisional data from 2022 indicate injuries, musculoskeletal diseases, and mental health disorders constitute the categories of medical conditions associated with the most medical encounters, largest number of affected service members, and greatest number of hospital days, consistent with previous burden reports. COVID-19 accounted for 1.4% of total active component service member medical encounters in 2022, a slight increase from the 1.2% rate in 2021. Only 0.3% of total hospital bed days in active component service members were for COVID-19 in 2022, an 83% drop from the 1.8% rate in 2021.
What is the impact on readiness and force health protection?
As in previous years, this report documents relatively few illnesses and injury categories that account for a substantial proportion of morbidity and health care burdens affecting U.S. active component service members. Preventable illnesses and injuries proven as disproportionate contributors to morbidity and health care burdens should be high priorities for intervention, research, and resources. Certain conditions that may affect readiness (e.g., pregnancy and maternal conditions) require scheduled, sustained care for optimal health, while other conditions such as injuries resulting from rigorous training for readiness, necessitate proven policies and safeguards to reduce injury rates while maintaining requisite training standards approved by senior leaders and commanders.
Methods
The population for this analysis includes all individuals who served in the active component of the Army, Navy, Air Force, or Marine Corps at any time during the surveillance period of January 1, 2022 through December 31, 2022. Each service member contributed encounters and person-time only for the actual months served during the surveillance period. All data in this analysis were derived from records maintained in the Defense Medical Surveillance System, which documents both ambulatory care encounters and hospitalizations of active component members of the U.S. Armed Forces. DMSS contains all encounters in military medical and civilian treatment facilities when reimbursed through the MHS. Encounters not routinely and completely documented within fixed military and non-military medical treatment facilities (e.g., during deployments, field training exercises, or at sea) are excluded from this analysis. This is the first year that DMSS data were housed and analyzed from the Military Health System Information Platform. Data quality assessments for completeness and timeliness are ongoing during the transition to MIP, and data presented in this report are considered provisional but current as of March 20, 2023.
DMSS data for all inpatient and outpatient medical encounters of active component service members during the surveillance period were summarized according to the primary (first-listed) diagnosis if reported with an ICD-10 code between A00 and T88, an ICD-10 code beginning with Z37 (outcome of delivery), or Department of Defense unique personal history codes DOD0101–DOD0105 (personal history of traumatic brain injury). All illness- and injury-specific diagnoses, as defined by ICD-10 codes, were grouped into 153 burden of disease-related “conditions” and 25 “categories” based on a modified version of the classification system developed for the GBD Study.1 This classification system was developed by the MSMR editorial staff in 2012 and is updated annually.
The GBD system groups diagnoses with common pathophysiologic or etiologic bases or significant DOD health policy importance. In this article, some diagnoses grouped into single categories in the GBD system (e.g., mental health disorders) were disaggregated to increase military relevance. In addition, injuries are classified by affected anatomic site rather than cause, as external causes of injuries using NATO Standardization Agreement (STANAG) 2050 codes are incompletely reported in military outpatient records.5
The morbidity burdens attributable to various conditions were estimated based on the total number of medical encounters associated with each condition, i.e., total hospitalizations and ambulatory visits for the condition with a limit of 1 encounter for an individual per condition each day; and numbers of service members affected by each condition, i.e., individuals with at least 1 medical encounter for the condition during the year; as well as total bed days during hospitalizations for each condition.
Results
Morbidity burden, by category
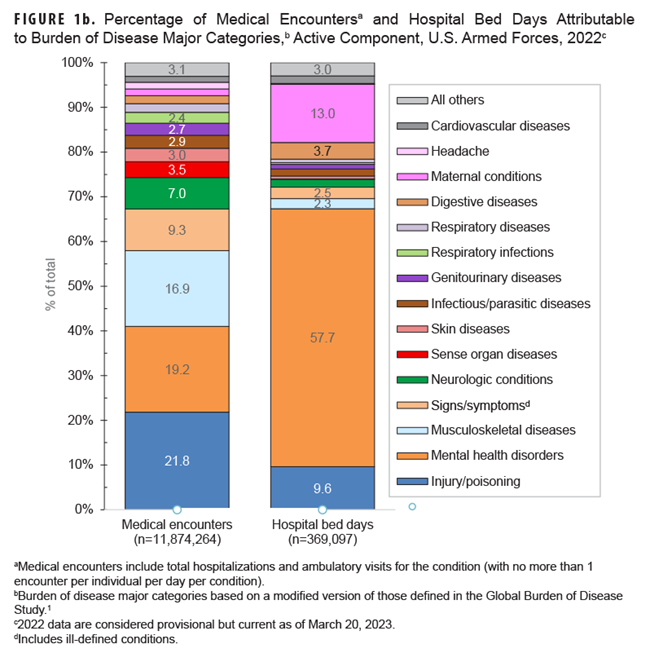
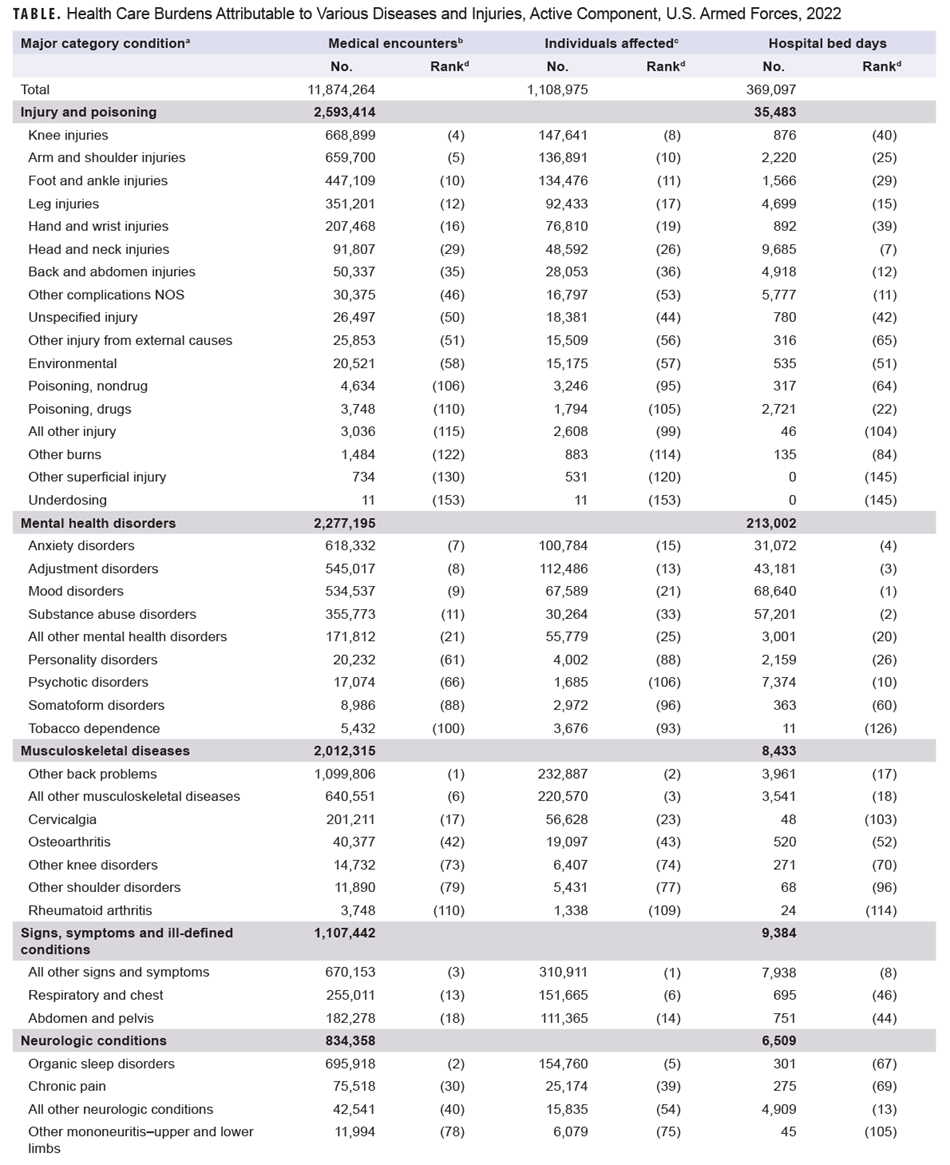
Provisional data indicate that in 2022 active component service members (individuals affected; n=508,355) experienced medical encounters due to injury more than any other morbidity-related category (Figure 1a).
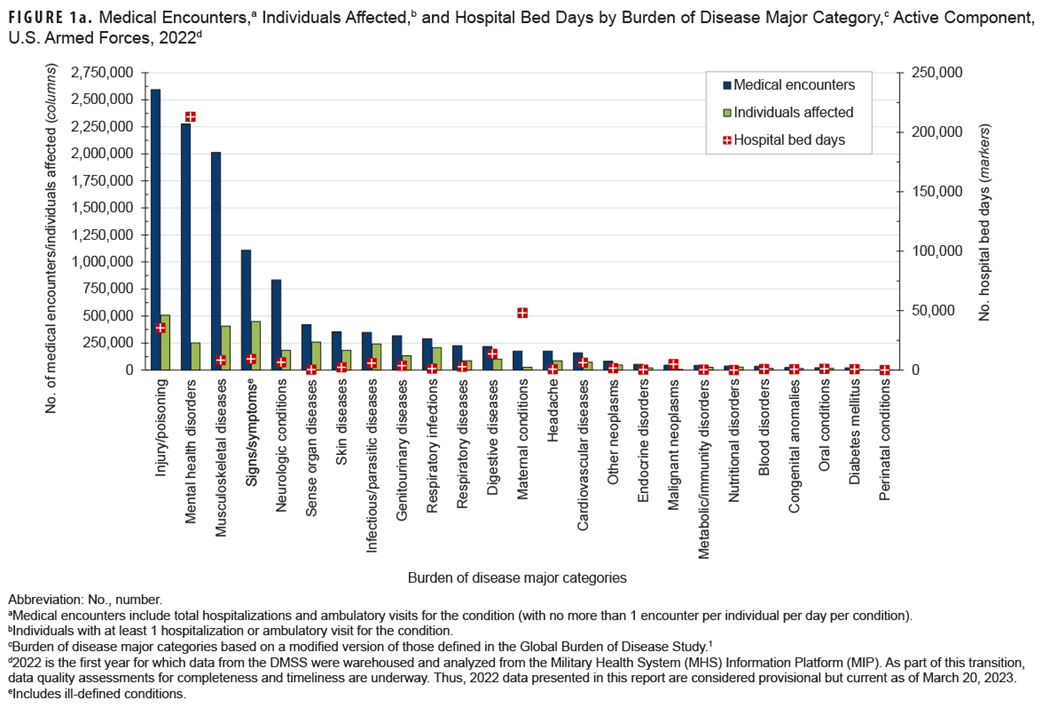
Ranking third in terms of hospital bed days, this major burden of disease category accounted for over one-fifth (21.8%) of all medical encounters (Figure 1b).
The injury category combines ICD-10 S (injury) and T codes (burns and poisonings); however, injuries account for nearly 90% of ambulatory encounters within the category (data not shown).6
Mental health disorders accounted for more hospital bed days (n=213,002) than any other morbidity-related category, contributing over half (57.7%) of all hospital bed days and ranking fifth for individuals affected (Figures 1a, 1b). Together, injury and mental health disorders accounted for over two-thirds (67.3%) of all hospital bed days and 41.0% of all medical encounters.
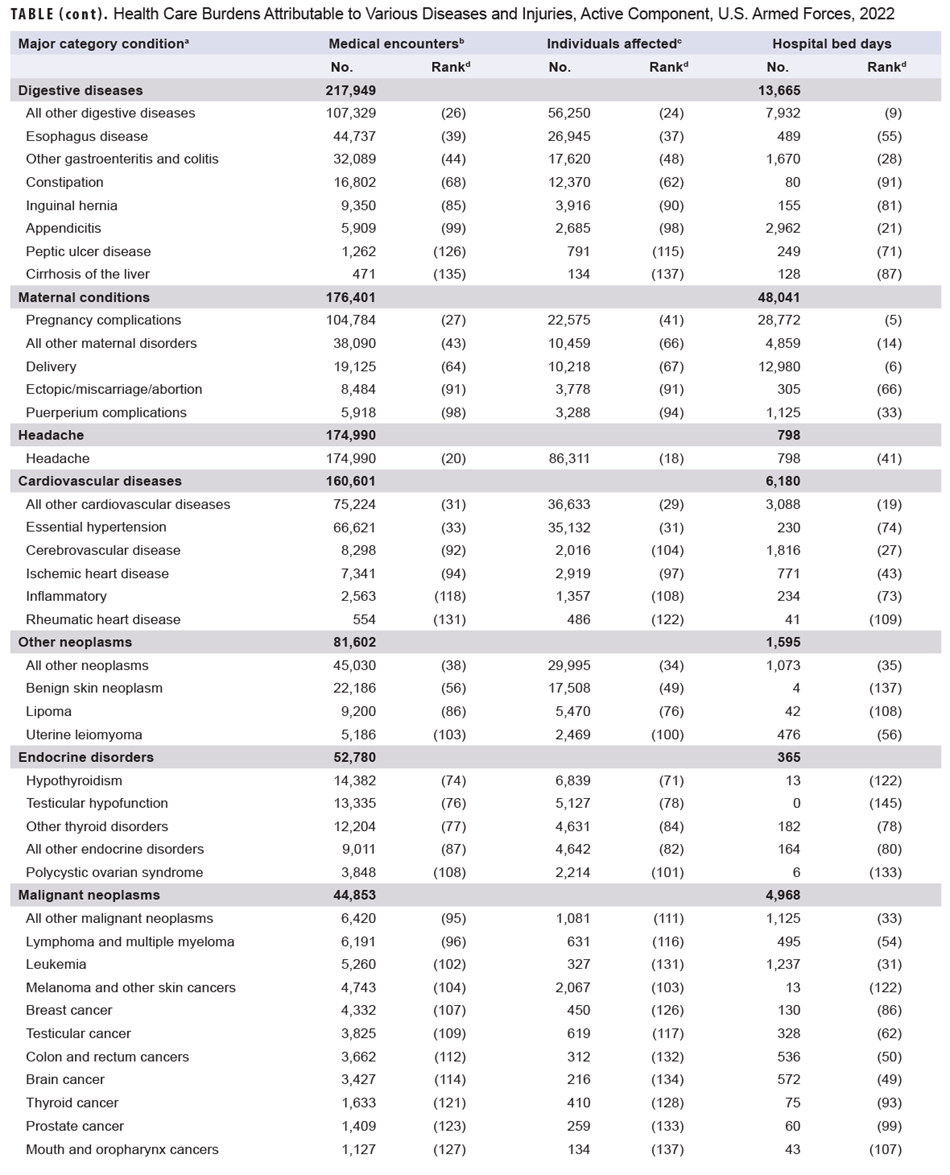
Maternal conditions (e.g., pregnancy complications and delivery) accounted for a relatively large proportion of all hospital bed days (n=48,041; 13.0%) but a much smaller proportion of medical encounters overall (n=176,401; 1.5 %) (Figures 1a, 1b). As women comprised only 17.5 % of the active duty force in 2022, these summary statistics understate the impact of these conditions among that group. Maternal conditions were the most frequent medical condition among active component women.
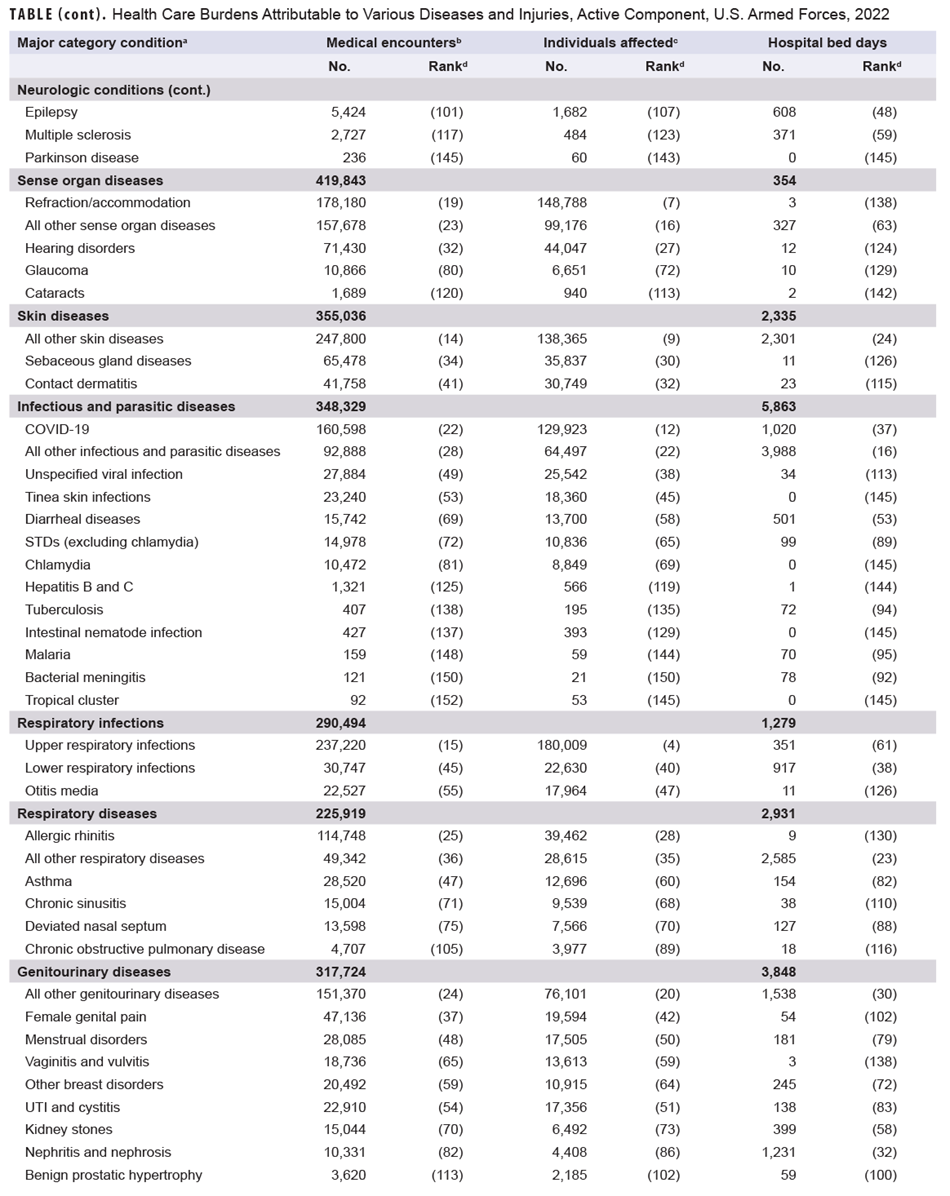
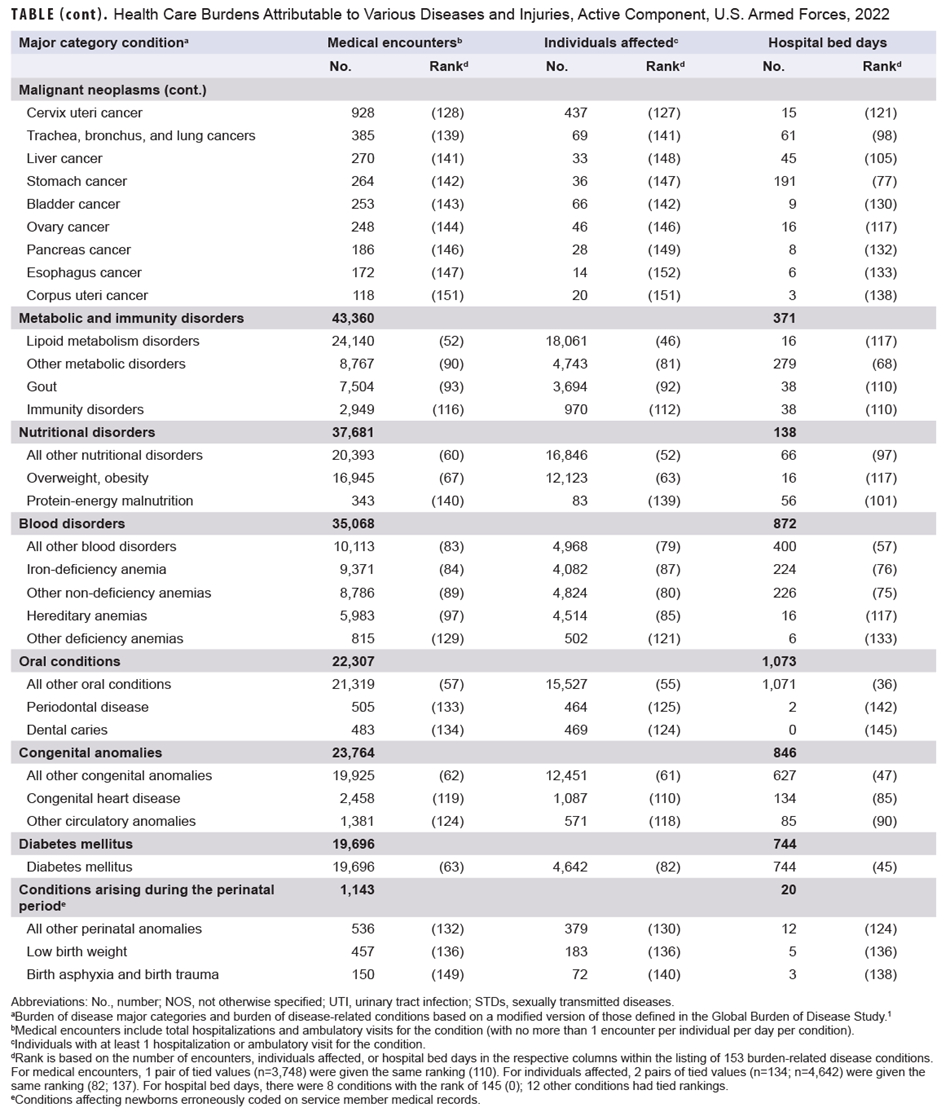
Medical encounters, by condition
In 2022, 5 burden of disease-related conditions accounted for almost one-third (32.0%) of all illness- and injury-related medical encounters: other back problems (e.g., low back pain, other dorsalgia); organic sleep disorders (e.g., insomnia, obstructive sleep apnea); all other signs and symptoms (e.g., fever, headache, general signs and symptoms not otherwise specified); knee injuries; and arm/shoulder injuries (Figure 2). Moreover, the 10 conditions associated with the most medical encounters constituted more than half (55.4%) of all illness- and injury-related medical encounters.
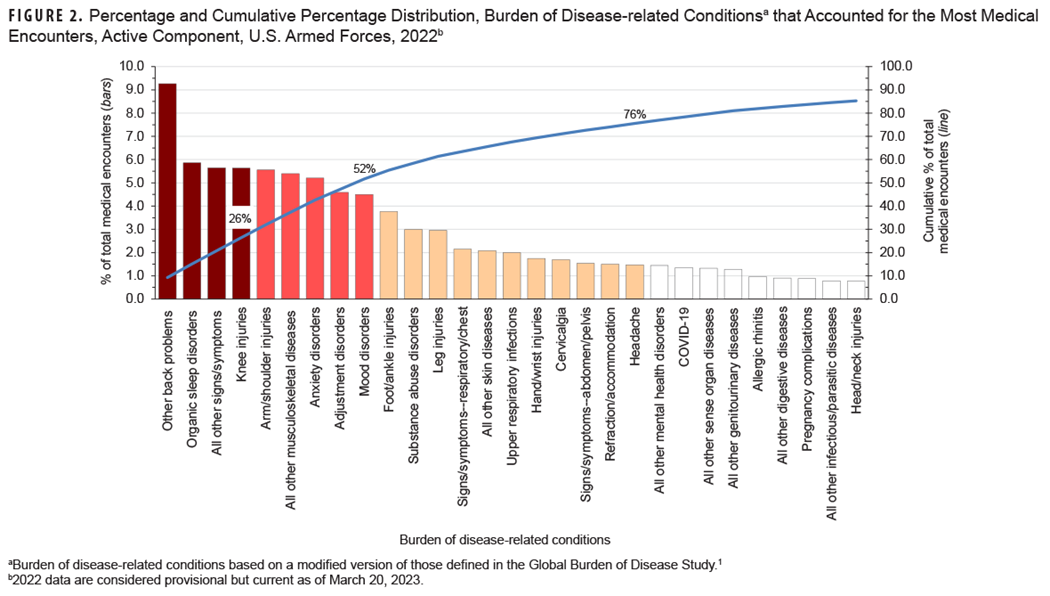
The health conditions that accounted for the most medical encounters among active component service members in 2022 were predominantly injuries, mental health disorders, and musculoskeletal diseases. Of the injuries reported in 2022, knee (5.6%), arm/shoulder (5.6%), foot/ankle (3.8%), and leg (3.0%) resulted in the most medical encounters (Figure 2, Table [at the bottom of the page]). The most frequent mental health disorder diagnoses resulted from anxiety (5.2%), adjustment (4.6%), mood (4.5%), and substance abuse disorders (3.0%). Other back problems (9.3%), all other musculoskeletal diseases (5.4%; e.g., pain in foot, pain in leg), and cervicalgia (1.7%) constituted the most medical encounters among musculoskeletal diseases. COVID-19 accounted for 1.4% of total medical encounters during 2022, a proportion nearly unchanged since 2021 (1.2%).
Individuals affected, by condition
In 2022, the 10 conditions that affected the most service members were all other signs and symptoms and respiratory/chest; other back problems and all other musculoskeletal diseases; knee and arm/shoulder injuries; upper respiratory infections; organic sleep disorders; refraction/accommodation disorders; and all other skin diseases. COVID-19 affected 129,923 service members, ranking 12th for number of service members affected in 2022, an increase in rank from 16th in 2021.
Hospital bed days, by condition
Mood and substance abuse disorders accounted for over one-third (34.1%) of all hospital bed days (Figure 3) experienced by active component members in 2022.
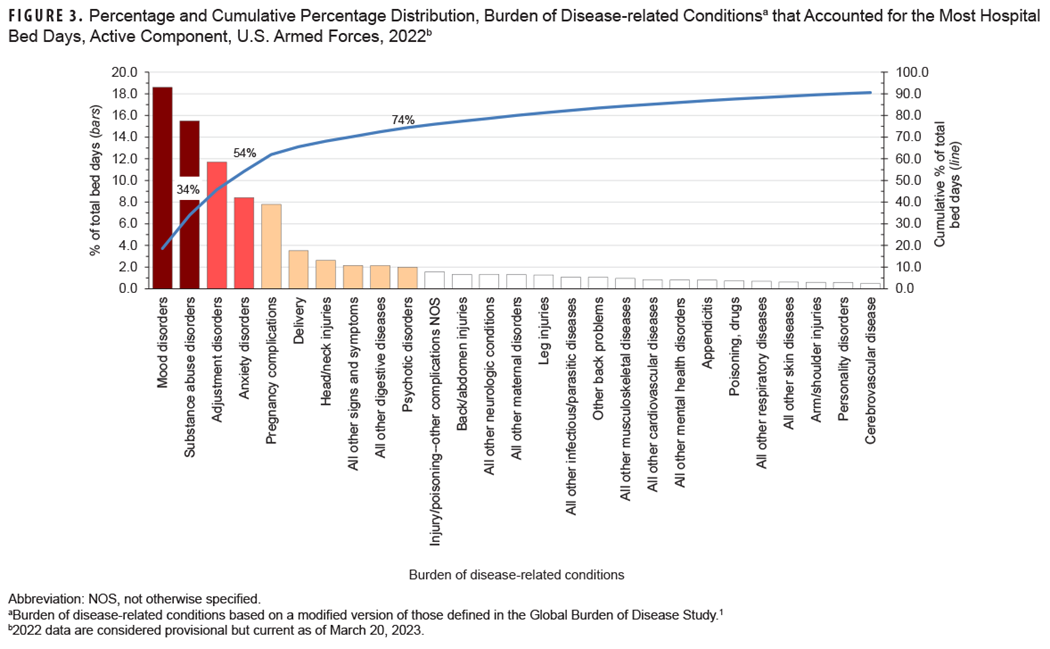
Four mental health disorders (mood, substance abuse, adjustment, and anxiety) and two maternal conditions (pregnancy complications and delivery) combined accounted for almost two-thirds (65.5%) of all hospital bed days (Table, Figure 3). About 10% of all hospital bed days in 2022 were attributable to injuries and poisonings. COVID-19 accounted for 0.3% of total hospital bed days in 2022 within the active component, down from 1.8% in 2021 (Table).
Relationships between health care burden indicators
There was a strong positive correlation between the number of medical encounters attributable to various conditions and the number of individuals affected by those conditions (r=0.87) (data not shown). The three leading causes of medical encounters were among the five conditions that affected the most individuals (Table). Meanwhile, weak to moderate positive relationships were determined for hospital bed days attributable to conditions and either numbers of individuals affected (r=0.20) by, or medical encounters associated (r=0.43) with, the same conditions. For example, substance abuse disorders and labor and delivery were among the top-ranking conditions by proportion of total hospital bed days, but these conditions affected relatively few active component service members in 2022.
Discussion
This report is consistent with the major findings of prior annual reports on morbidity and health care burdens among U.S. military members. Mental health disorders (including substance abuse disorders), injuries, and musculoskeletal disorders of the back have been leading causes of morbidity and disability among service members throughout military history.7-13 It is well-recognized that the prevention, treatment, and rehabilitation of back problems and joint injuries, and the detection, characterization, and management of mental health disorders—including substance abuse and deployment stress-related disorders (e.g., post-traumatic stress disorder)—should be the highest priorities for military medical research, public health, and force health protection programs.
In a given population and setting, the classification system or measure utilized to quantify condition-specific morbidity burdens determines conclusions about the relative importance of various conditions and, in turn, resources allocated for their treatment. The additional visits due to readiness requirements may be administrative or a consequence of a training or occupational injury. There is an interest among senior leaders and policymakers in the “cost of readiness,” and an ideal burden of disease classification scheme for the military population would enable identification of readiness-related visits.
In 2022, consistent with previous reports, the burden of disease major categories of injury, musculoskeletal diseases, mental health disorders, and maternal conditions accounted for relatively large proportions of the morbidity and health care burdens that affected active component service members. Only 9 (5.9%) of the 153 burden of disease-related conditions accounted for slightly more than half of all illness- and injury-related medical encounters: These conditions included two musculoskeletal conditions (other back problems and all other musculoskeletal diseases), two anatomic site-defined injuries (knee and arm/shoulder), organic sleep disorders, all other signs and symptoms, and three mental health disorders (anxiety, adjustment, and mood disorders). This pattern of illness and injury among U.S. active component members is distinct from other population groups with different demographic distributions and occupational hazards, such as the general U.S. population and non-service member MHS beneficiaries; differing burdens of disease and injury for non-service member MHS beneficiaries will be described in the July 2023 MSMR. As noted, the data presented in this report are considered provisional, and ongoing inquiries regarding data completeness in the MHS MIP may result in later updates to the patterns of morbidity and health care burden reported here.
Although 2022 was affected by the COVID-19 pandemic, COVID-19 accounted for relatively modest numbers of medical encounters and bed days compared to other conditions in this analysis, likely due to several factors, among them the fact that active component service members represent a relatively young and healthy population. The unique coding scheme for COVID-19 may also mask its true impact. COVID-19 encounters have a special purpose ICD-10 code (U07.1) not included with other infectious diseases. The number of ambulatory encounters for COVID-19 alone was nearly equal to the total ambulatory encounters for all infectious diseases (ICD codes A and B). It is possible some COVID-19 encounters were coded under either infectious diseases, acute respiratory infections (ICD-10 codes J00-J06), or other general symptoms and signs (ICD-10 code R68.89). ICD-10 code U07.1 may have been used as a secondary code, or not at all, for some COVID-19 encounters.
References
- Murray CJL, Lopez AD, eds. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press, 1996:120-122.
- World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization, 2008.
- Defense Manpower Data Center. Self-Service Reports, Active Duty by Demographics, Service Branch. Accessed June 15, 2023. https://dmdcrs.dmdc.osd.mil/dmdcrs/public
- United States Census Bureau. Age and Sex Composition in the United States: 2021. Table 1: Population by Age and Sex. Accessed June 15, 2023. https://www.census.gov/data/tables/2021/demo/age-and-sex/2021-age-sex-composition.html
- Armed forces Health Surveillance Branch. Hospitalizations, active component, U.S. Armed Forces, 2019. MSMR. 2020;27(5):10-17.
- Armed Forces Health Surveillance Division. Ambulatory visits, active component, U.S. Armed Forces, 2022. MSMR. 2023;29(6):19-25.
- Packnett ER, Elmasry H, Toolin CF, Cowan DB, Boivin MR. Epidemiology of major depressive disorder disability in the US military: FY 2007–2012. J Nerv Ment Dis. 2017;205(9):672-678.
- Moradi Y, Dowran B, Sepandi M. The global prevalence of depression, suicide ideation, and attempts in the military forces: a systematic review and meta-analysis of cross sectional studies. BMC Psychiatry. 2021;21(1):510. doi:10.1186/s12888-021-03526-2
- Stahlman S, Oetting AA. Mental health disorders and mental health problems, active component, U.S. Armed Forces, 2007–2016. MSMR. 2018;25(3):2-11.
- Update: Mental health disorders and mental health problems, active component, U.S. Armed Forces, 2016–2020. MSMR. 2021;28(8)2-9.
- Jones BH, Perrotta DM, Canham-Chervak ML, Nee MA, Brundage JF. Injuries in the military: a review and commentary focused on prevention. Am J Prev Med. 2000;18(3 suppl):71-84.
- Lovalekar M, Hauret K, Roy T, et al. Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. J Sci Med Sport. 2021;24(10):963-969. doi: 10.1016/j.jsams.2021.03.016
- To D, Razai M, Murnaghan K, Cancelliere, C. Risk factors for low back pain in active military personnel: a systematic review. Chiropr Man Therap. 2021 Dec 30;29(1):52. doi:10.1186/s12998-021-00409-x