The 2022-2025 National HIV/AIDS Strategy to end the HIV epidemic by 2030 includes an implementation plan that directs the Department of Defense (DOD) to “continue to implement interventions, testing, education, and training on the prevention of transmission of HIV infection as described in DODI [DOD Instruction] 6485.01, DHA-PI [Defense Health Agency-Procedural Instruction] 6025.29, and DHA-PI 6485.01.”1,2
The annual crude rate of new HIV infections in the U.S. military between 2018 and 2023 was 21 per 100,000 population,3 much higher than the estimated 11.5 per 100,000 in the U.S. general population in 2021.4 A comparison of U.S. military and general population rates of HIV infection, adjusted for relevant confounding variables, has not been published, neither for U.S. military HIV incidence rates among different races and ethnicities. This Surveillance Snapshot presents a comparison of U.S. active component military and general population HIV incidence rates in 2021,4 the most recent year for which stratified U.S. data were available, using indirect standardization by sex, age, and race and ethnicity.
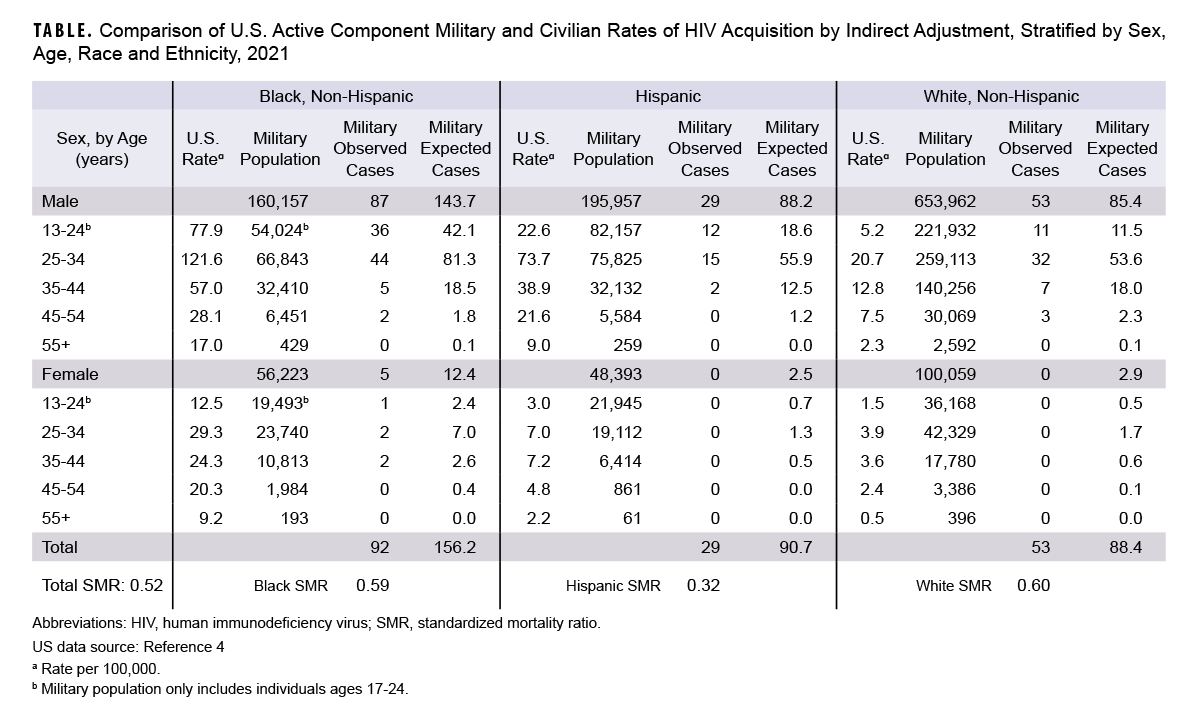
There were 174 observed cases of HIV in the U.S. military in 2021 who self-identified their race and ethnicity as Black, Hispanic, or White, compared to an expected number of 335 based on U.S. population rates,5 resulting in an overall standardized morbidity ratio of 0.52 (Table). The rate of HIV in the active component U.S. military was 48% lower than the U.S. general population rate after adjusting for sex, age, and race and ethnicity. SMR estimates stratified by race and ethnicity were similar for non-Hispanic Black and White service members (0.59 and 0.60, respectively) but lower for Hispanic service members (SMR=0.32). SMRs for racial and ethnic groups other than White, Black, and Hispanic cannot be presented because U.S. general population rates have not been not published for additional groups.4
Since the U.S. military requires HIV testing at least biennially,6 it is unlikely that significant numbers of cases in the U.S. military are being missed, whereas infected individuals might be undiagnosed for longer periods of time in the general population if untested, leading to underestimates in younger populations.
The findings from this Snapshot may help to contextualize lower use (24%) of HIV pre-exposure prophylaxis in 2021 among those in the U.S. military with indications for its use, published in this issue of the MSMR,7 compared to those at risk in the general population (30%). The lower adjusted U.S. military rate of HIV infection may be due to unmeasured behavioral or other factors rather than increased use of PrEP. These findings are consistent with the presence of a selection bias (or ‘healthy warrior effect’) resulting from the exclusion of HIV-infected individuals from entry into service,8 as some of those with higher-risk sexual behaviors would have already been infected. Despite the lower adjusted rate of HIV infection in the U.S. military, HIV remains a threat to force health protection due to its costs, health consequences, and impact on military readiness.9
Author Affiliations
Uniformed Services University Department of Preventive Medicine and Biostatistics: Dr. Mancuso; Epidemiology and Analysis Branch, Armed Forces Health Surveillance Division, Defense Health Agency: Dr. Mabila
Disclaimer
The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, assertions, opinions, nor policies of the Uniformed Services University of the Health Sciences, the Defense Health Agency, or the Department of Defense.
References
- The White House. National HIV/AIDS Strategy for the United States 2022-2025. Accessed Jul. 9, 2023. https://files.hiv.gov/s3fs-public/NHAS-2022-2025.pdf
- The White House. National HIV/AIDS Strategy Federal Implementation Plan. Updated Aug. 21, 2023. Accessed Nov. 4, 2023. https://www.hiv.gov/federal-response/national-hiv-aids-strategy/implementing-national-hiv-aids-strategy
- Armed Forces Health Surveillance Division. Update: routine screening for antibodies to human immunodeficiency virus, U.S. Armed Forces, active and reserve components, January 2018-June 2023. MSMR. 2023;30(9):2-10.
- Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States 2017-2021. Updated May 23, 2023. Accessed Nov. 4, 2023. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-28-no-3/index.html
- Inskip H, Beral V, Fraser P, Haskey J. Methods for age-adjustment of rates. Stat Med. 1983;2(4):455-466. doi:10.1002/sim.4780020404
- Under Secretary of Defense for Personnel and Readiness. DOD Instruction 6485.01: Human Immunodeficiency Virus (HIV) in Military Service Members. Department of Defense. Updated Jun. 6, 2022. Accessed Nov. 4, 2023. https://www.esd.whs.mil/portals/54/documents/dd/issuances/dodi/648501p.pdf
- Mancuso JD, Ahmed AE. Coverage of HIV pre-exposure prophylaxis (PrEP) in the active duty U.S. military, 2023. MSMR. 2024;31(3):13-16.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6130.03, Volume 1. Medical Standards for Military Service: Appointment, Enlistment, or Induction. Department of Defense. Updated Nov. 16, 2022. Accessed Jul. 7, 2023. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/613003_vol1.PDF?ver=7fhqacc0jGX_R9_1iexudA%3D%3D
- Cavanaugh JS, Murray CK, Chang D, Ake JA. The purpose and impact of the U.S. military HIV research program. JFQ. 2023;110(3rd quarter):69-74.