What Are the New Findings?
From Jan. 2015 through June 2020, the rates of HIV test positivity among civilian applicants for military service were stable at 0.32 per 1,000 tested. Among uniformed personnel (active component, Guard, and reserve), rates since 2015 decreased or remained relatively stable. Rates among female applicants and female service members have remained very low compared to those of males.
What Is the Impact on Readiness and Force Health Protection?
The routine screening for antibodies to HIV for over 30 years has enabled the U.S. military to provide to infected service members adequate and timely medical evaluations, treatments, counseling to prevent unwitting transmission, and protection of the battlefield blood supply.
Abstract
This report provides an update through June 2020 of the results of routine screening for antibodies to the human immunodeficiency virus (HIV) among civilian applicants for military service and among members of the active and reserve components of the U.S. Armed Forces. During Jan. 2015– June 2020, full-year seroprevalences among applicants for service remained stable and ranged from 0.30 to 0.34 per 1,000 tested. Seroprevalences also peaked in 2015 for active component service members of the Army, Navy, and Air Force and among reservists of the Navy and Marine Corps. Overall, across the services, HIV-antibody seroprevalences were highest among Army reservists, Army National Guard members, and Navy reservists and lowest among Air National Guard members, Marine Corps active component members, and Air Force reservists. Across active and reserve components of all services, HIV-antibody seroprevalences continued to be higher among men than women.
Background
Since acquired immune deficiency syndrome (AIDS) was first recognized as a distinct clinical entity in 1981,1 its spread has had major impacts on the health of populations and on health care systems worldwide. Human immunodeficiency virus type 1 (HIV-1) was identified as the cause of AIDS in 1983. For more than 30 years, the U.S. military has conducted routine screening for antibodies to HIV-1 to enable adequate and timely medical evaluations, treatment, and counseling; to prevent unwitting transmission; and to protect the battlefield blood supply.
As part of the U.S. military's total-force HIV screening program, civilian applicants for military service are screened for antibodies to HIV during pre-accession medical examinations. Infection with HIV is medically disqualifying for entry into U.S. military service.4 Since 1986, all members of the active and reserve components of the U.S. Armed Forces have been periodically screened to detect newly acquired HIV infections. In 2004, the Department of Defense (DOD) set a standard testing interval of 2 years for all service members.5,6 All military personnel are periodically screened for HIV infection (at a minimum every 2 years or before deployment, on return from deployment, or after having received a diagnosis of various other conditions, such as a sexually transmitted infection).6 Routine HIV screenings are usually performed during the Periodic Health Assessment, an annual evaluation of a service member medical readiness status. Service members who are infected with HIV receive clinical assessments, treatments, and counseling; they may remain in service as long as they are able to fully perform their military duties.2,3 HIV+ service members continue to be eligible for certain noncombat or noncontingency deployments and, as such, must meet the DOD's retention policy for non-deployable service members. The latest policy on retention determinations for non-deployable service members was implemented in Oct. 2018 and requires service members who are in a non-deployable status for more than 12 consecutive months to be evaluated for a retention determination by their respective military departments or, as appropriate, be referred into the Disability Evaluation System, or be processed for administrative separation from the military.7
Before 2009, all of the aforementioned screening programs used laboratory techniques that detected only HIV-1–type infections. Starting in 2009, all programs adopted methods that allowed the detection of antibodies to both major HIV types (i.e., HIV-1 and HIV-2). Although HIV-2 infection is rare in the U.S. and no instances of HIV-2 infection have thus far been detected in civilian applicants or service members since 2009, HIV-2 is much more prevalent in other parts of the world where service members may be required to serve. To provide for the change in laboratory methods in the past and for the prospect of future detections of HIV-2 infection in the services' screening programs, this report will hereafter refer to the target of the screening programs as simply "HIV" without specifying the types.
This report summarizes numbers, seroprevalences, and trends of newly identified HIV-antibody positivity among civilian applicants for military service and members of the active and reserve components of the U.S. Armed Forces from 1 Jan. 2015 through 30 June 2020. Summaries of results of routine screening for antibodies to HIV among civilian applicants and active and reserve component members of the U.S. military since 1990 are available at www.health.mil/MSMRArchives.
Methods
The surveillance period was 1 Jan. 2015 through 30 June 2020. The surveillance population included all civilian applicants for U.S. military service and all individuals who were screened for antibodies to HIV while serving in the active or reserve component of the Army, Navy, Air Force, or Marine Corps during the surveillance period
All individuals who were tested and all first-time detections of antibodies to HIV through U.S. military medical testing programs were ascertained by matching specimen numbers and serologic test results to the personal identifiers of providers of the specimens. With the exception of U.S. Air Force members, all results were accessed from records routinely maintained in the Defense Medical Surveillance System (DMSS). The U.S. Air Force provided summarized results of serologic screening for antibodies to HIV among its members.
An incident case of HIV-antibody seropositivity was defined as 2 positive results from serologic testing of 2 different specimens from the same individual or 1 positive result from serologic testing of the most recent specimen provided by an individual
Annual prevalences of HIV seropositivity among civilian applicants for service were calculated by dividing the number of applicants identified as HIV-antibody seropositive during each calendar year by the number of applicants tested during the corresponding year. For annual HIV seroprevalence summaries among U.S. service members, denominators were the numbers of individuals in each component of each service branch who were tested at least once during the relevant calendar year.
Results
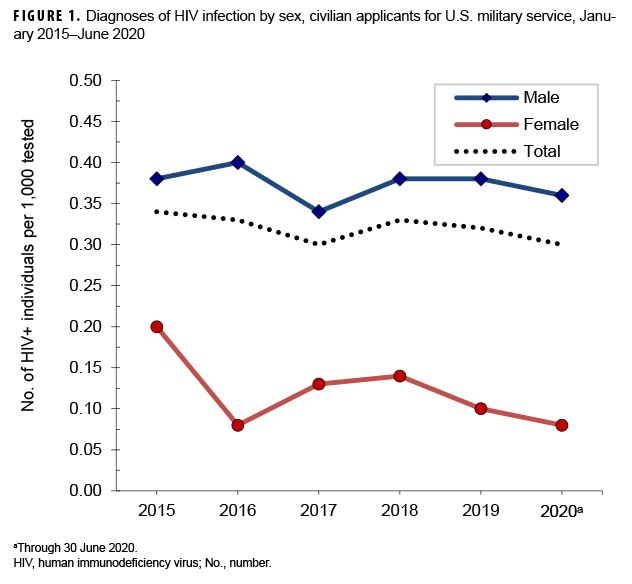
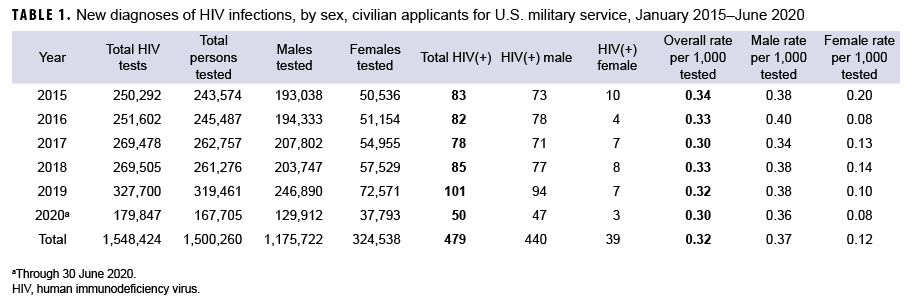
Civilian applicants
From Jan. 2019 through June 2020, a total of 487,166 civilian applicants for U.S. military service were tested for antibodies to HIV, and 151 applicants were identified as HIV -antibody positive (seroprevalence: 0.31 per 1,000 applicants tested)(Table 1). During the surveillance period, full-year seroprevalences among applicants for service were highest in 2015 (0.34 per 1,000 tested) and then decreased during the subsequent 2 years (0.33 and 0.30 per 1,000 tested, respectively) (Table 1, Figure 1). In 2018, the seroprevalence increased slightly to 0.33 per 1,000 tested and then remained relatively stable at 0.32 per 1,000 tested in 2019.
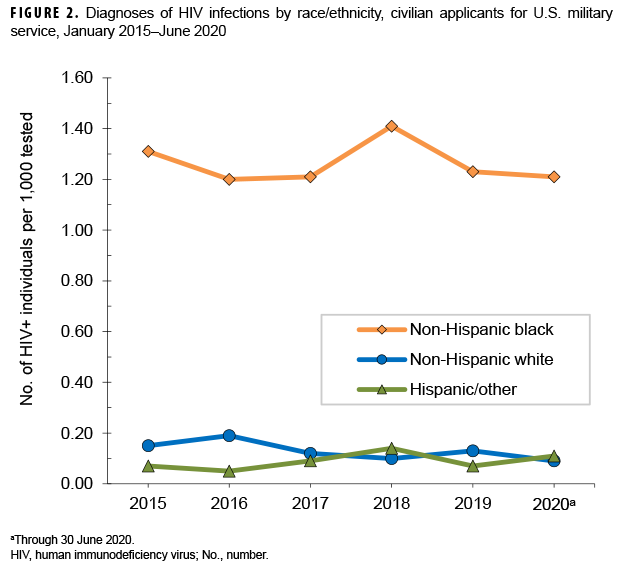
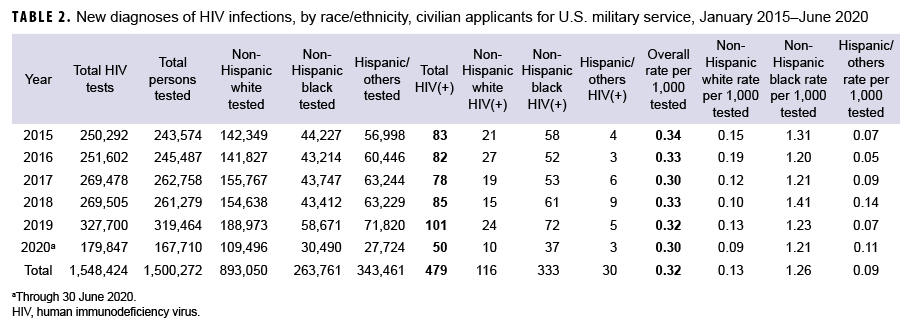
Throughout the surveillance period, annual HIV-antibody seroprevalences among male applicants were consistently higher than among female applicants (Table 1, Figure 1). Seroprevalences were much higher among non-Hispanic blacks, compared with other race/ethnicity groups (Table 2, Figure 2). During 2019, on average, 1 civilian applicant for service was detected with antibodies to HIV per 3,245 screening tests (Table 1).
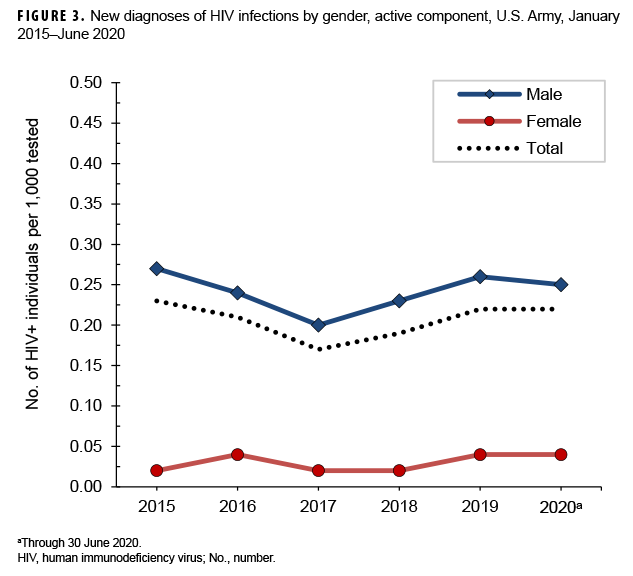
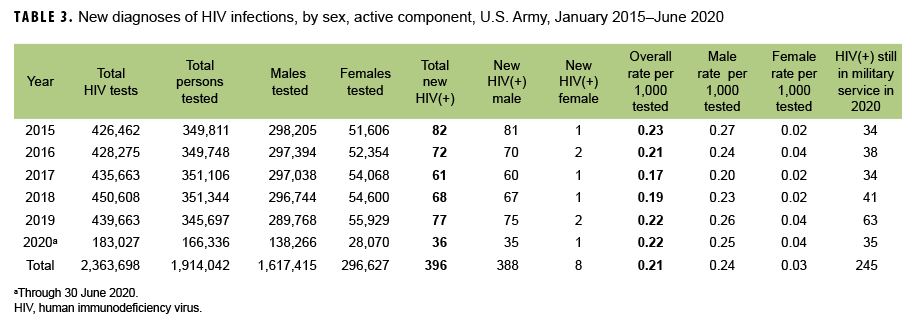
U.S Army
Active component: From Jan. 2019 through June 2020, a total of 512,033 soldiers in the active component of the U.S. Army were tested for antibodies to HIV, and 113 soldiers were identified as HIV antibody positive (seroprevalence: 0.22 per 1,000 soldiers tested) (Table 3). During the surveillance period, annual seroprevalences fluctuated between a low of 0.17 per 1,000 tested in 2017 and a high of 0.23 per 1,000 tested in 2015 (Table 3, Figure 3). Annual seroprevalences for male active component Army members were considerably higher than those of females (Figure 3). During 2019, on average, 1 new HIV infection was detected among active component Army soldiers per 5,710 screening tests (Table 3). Of the 396 active component soldiers diagnosed with HIV infections since 2015, a total of 245 (61.9%) were still in military service in 2020.
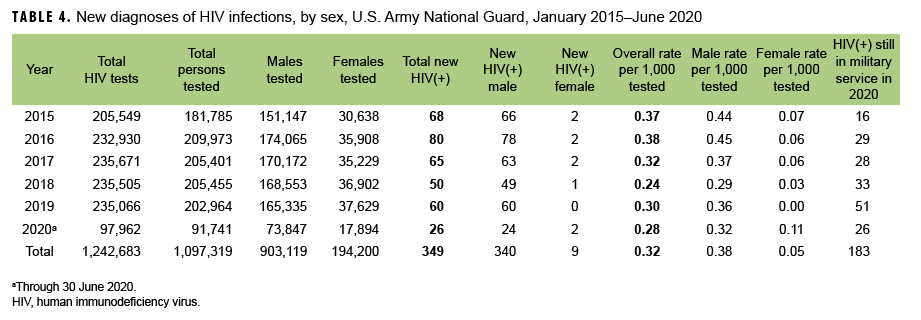
Army National Guard: From Jan. 2019 through June 2020, a total of 294,705 members of the U.S. Army National Guard were tested for antibodies to HIV, and 86 soldiers were identified as HIV antibody positive (seroprevalence: 0.29 per 1,000 soldiers tested) (Table 4). Among Army National Guard soldiers, annual seroprevalences decreased markedly from 2016 through 2018 (seroprevalences: 0.38 and 0.24 per 1,000 soldiers tested, respectively), increased in 2019 (0.30 per 1,000 tested), and then decreased slightly in the first 6 months of 2020 (0.28 per 1,000 tested). On average, during 2019, 1 new HIV infection was detected among Army National Guard soldiers per 3,918 screening tests. Of the 349 National Guard soldiers who tested positive for HIV since 2015, a total of 183 (52.4%) were still in military service in 2020.
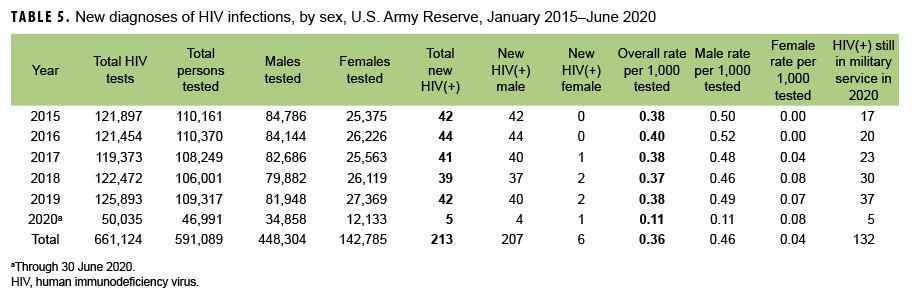
Army Reserve: From Jan. 2019 through June 2020, a total of 156,308 members of the U.S. Army Reserve were tested for antibodies to HIV, and 47 soldiers were identified as HIV antibody positive (seroprevalence: 0.30 per 1,000 soldiers tested) (Table 5). Among Army reservists during the surveillance period, seroprevalence was highest in 2016 at 0.40 per 1,000 tested, decreased slightly in 2017 to 0.38 per 1,000 tested, and then remained relatively stable through 2019. This pattern was followed by a considerable decrease in seroprevalence in the first 6 months of 2020 (0.11 tested per 1,000). During 2019, on average, 1 new HIV infection was detected among Army reservists per 2,997 screening tests (Table 5). Of the 213 Army reservists diagnosed with HIV infections since 2015, a total of 132 (62.0%) were still in military service in 2020.
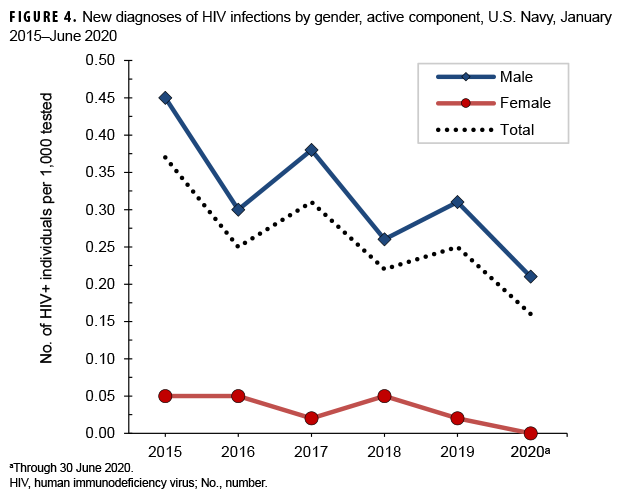
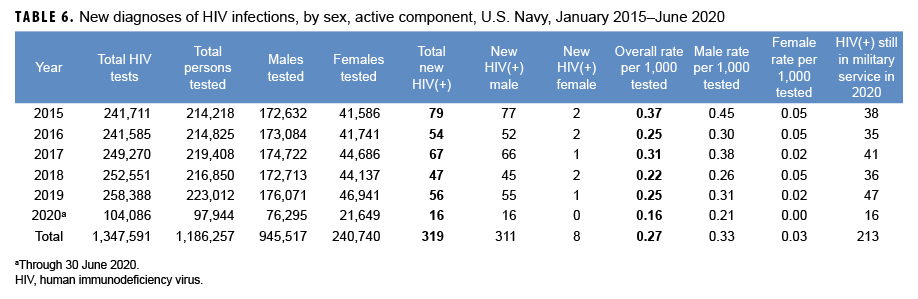
U.S. Navy
Active component: From Jan. 2019 through June 2020, a total of 320,956 active component members of the U.S. Navy were tested for antibodies to HIV, and 72 sailors were identified as HIV antibody positive (seroprevalence: 0.22 per 1,000 sailors tested) (Table 6). Among tested male active component sailors, full-year annual HIV-antibody seroprevalences decreased 30.0% between 2015 and 2019 (Figure 4). Annual seroprevalences remained relatively low and stable among female sailors during the surveillance period. During 2019, on average, 1 new HIV infection was detected among active component sailors per 4,614 screening tests (Table 6). Of the 319 active component sailors who tested positive for HIV since 2015, a total of 213 (66.8%) were still in military service in 2020.
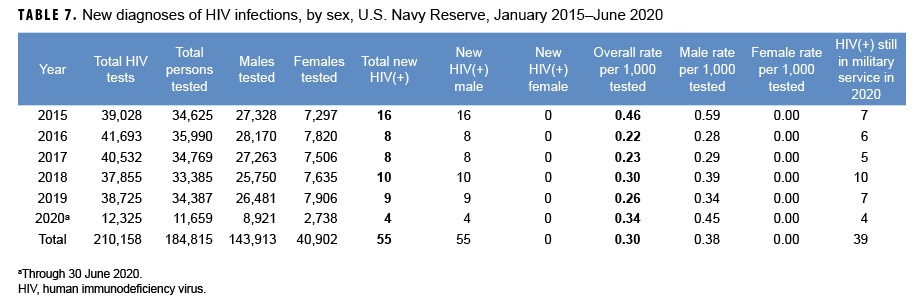
Navy Reserve: From Jan. 2019 through June 2020, a total of 46,046 members of the U.S. Navy Reserve were tested for antibodies to HIV, and 13 sailors were identified as HIV antibody positive (seroprevalence: 0.28 per 1,000 sailors tested) (Table 7). The HIV-antibody seroprevalence among Navy reservists in 2015 was more than 2 times that in 2016 (seroprevalences: 0.46 and 0.22 per 1,000 sailors tested, respectively). Since 2007, no female Navy reservist has been detected with antibodies to HIV during routine testing (data not shown). On average, during 2019, 1 new HIV infection was detected among Navy reservists per 4,303 screening tests (Table 7). Of the 55 reserve component sailors diagnosed with HIV infections since 2015, a total of 39 (70.9%) were still in military service in 2020.
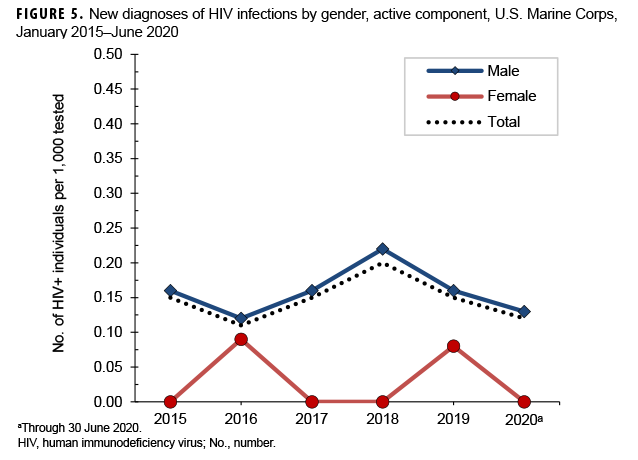
U.S. Marine Corps
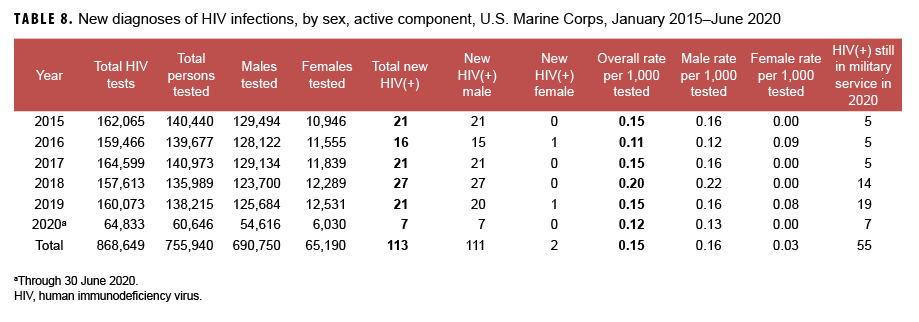
Active component: From Jan. 2019 through June 2020, a total of 198,861 members of the active component of the U.S. Marine Corps were tested for antibodies to HIV, and 28 Marines were identified as HIV antibody positive (seroprevalence: 0.14 per 1,000 Marines tested) (Table 8). From Jan. 2015 through June 2020, seroprevalences of antibodies to HIV remained relatively low and stable among routinely tested Marines (Figure 5). During 2019, on average, 1 new HIV infection was detected among active component Marines per 7,623 screening tests (Table 8). Of the 113 active component Marines diagnosed with HIV infections since 2015, a total of 55 (48.7%) were still in military service in 2020.
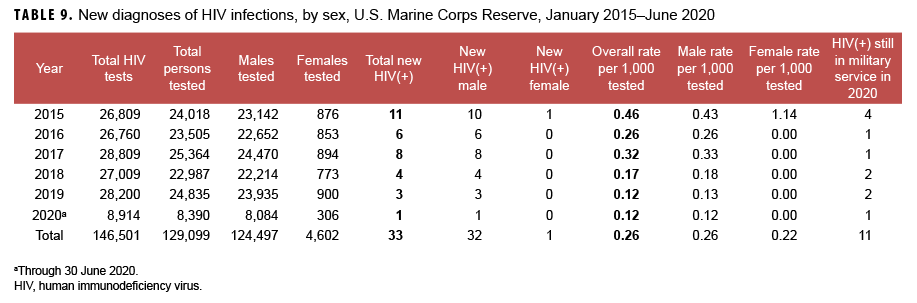
Marine Corps Reserve: From Jan. 2019 through June 2020, a total of 33,225 members of the U.S. Marine Corps Reserve were tested for antibodies to HIV, and 4 Marine Corps reservists were identified as HIV antibody positive (seroprevalence: 0.12 per 1,000 Marines tested) (Table 9). During the surveillance period, seroprevalences among Marine Corps reservists peaked at 0.46 per 1,000 tested in 2015, and reached a low of 0.12 per 1,000 tested in 2019, and remained stable through June 2020. From 1990 through June 2020, only 1 female Marine Corps reservist was detected with antibodies to HIV during routine screening (data not shown). During 2019, on average, 1 new HIV infection was detected among Marine Corps reservists per 9,400 screening tests (Table 9). Of the 33 Marine Corps reservists diagnosed with HIV infection since 2015, a total of 11 (33.3%) were still in military service in 2020.
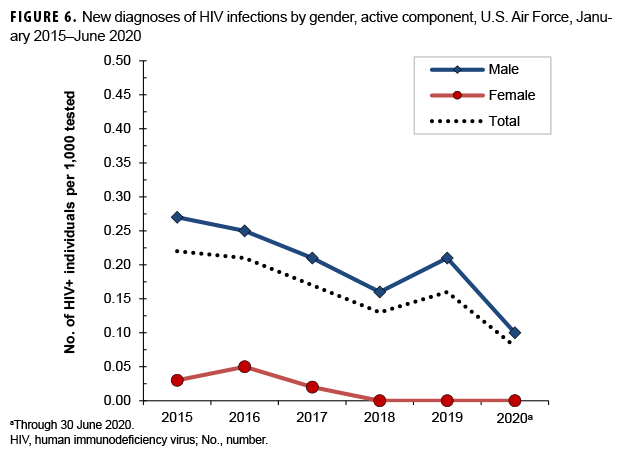
U.S. Air Force
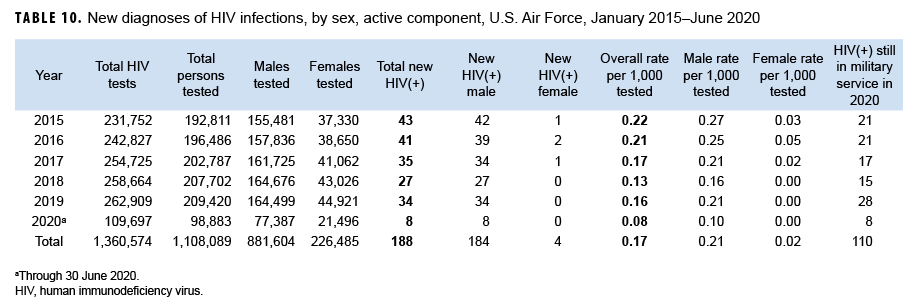
Active component: From Jan. 2019 through June 2020, a total of 308,303 active component members of the U.S. Air Force were tested for antibodies to HIV, and 42 airmen were diagnosed with HIV infections (seroprevalence: 0.14 per 1,000 airmen tested) (Table 10). During the surveillance period, seroprevalences among males ranged from a high of 0.27 per 1,000 tested in 2015 to a low of 0.10 per 1,000 tested in the first 6 months of 2020 (Figure 6). Among females during the surveillance period, annual seroprevalences remained relatively low and stable. During 2019, on average, 1 new HIV infection was detected among active component Air Force members per 7,733 screening tests (Table 10). Of the 188 active component airmen diagnosed with HIV infections since 2015, 110 (58.5%) were still in military service in 2020.
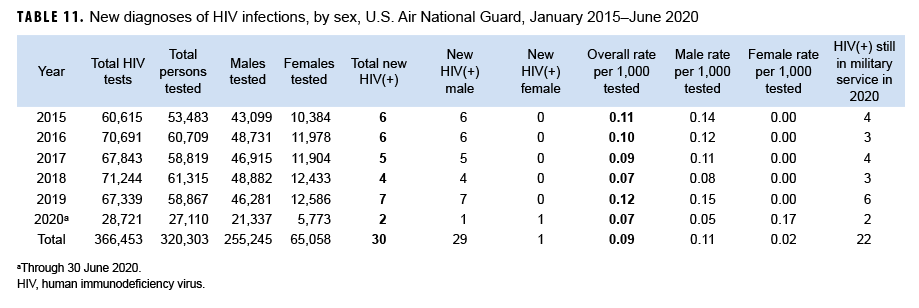
Air National Guard: From Jan. 2019 through June 2020, a total of 85,977 members of the Air National Guard were tested for antibodies to HIV, and 9 airmen were diagnosed with HIV infections (seroprevalence: 0.10 per 1,000 airmen tested) (Table 11). In the first 6 months of 2020, 1 female Air National Guard member was detected with antibodies to HIV, the first since 2010 (data not shown). During 2019, on average, 1 new HIV infection was detected among Air National Guard members per 9,620 screening tests (Table 11). Of the 30 Air National Guard members diagnosed with HIV infections since 2015, 22 (73.3%) were still in military service in 2020.
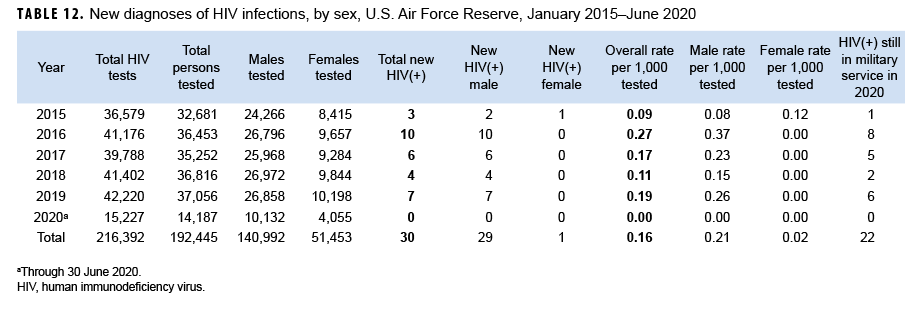
Air Force Reserve: From Jan. 2019 through June 2020, a total of 51,243 members of the Air Force Reserve were tested for antibodies to HIV, and 7 airmen were diagnosed with HIV infections (seroprevalence: 0.14 per 1,000 airmen tested) (Table 12). During 2019, on average, 1 new HIV infection was detected among Air Force reservists per 6,031 screening tests (Table 12). Of the 30 reserve component airmen diagnosed with HIV infections since 2015, 22 (73.3%) were still in military service in 2020.
Editorial Comment
The U.S. military has conducted routine screening for antibodies to HIV among all civilian applicants for service and all active and reserve component members of the services for more than 30 years.2,3,5,6 Results of U.S. military HIV antibody testing programs have been summarized in the MSMR for more than 2 decades.8
This report documents that, since 2015, prevalences of HIV seropositivity among civilian applicants for military service have fluctuated between 0.30 per 1,000 tested in 2017 and 0.34 per 1,000 applicants tested in 2015. It is important to note that because applicants for military service are not randomly selected from the general population of U.S. young adults, seroprevalences among applicants are not directly indicative of HIV prevalences, infection rates, or trends in the U.S. civilian population. As such, relatively low prevalences of HIV among civilian applicants for military service do not necessarily indicate low prevalences or incidence rates of HIV among young adults in the U.S. in general.
This report also documents that full-year HIV-antibody seroprevalences among members of the active components ranged from 0.11 per 1,000 tested (Marine Corps, 2016) to 0.37 per 1,000 tested (Navy, 2015). Full-year seroprevalences among the Reserve/Guard components fluctuated between 0.07 per 1,000 tested (Air National Guard, 2018) and 0.46 per 1,000 tested (Navy Reserve, 2015; Marine Corps Reserve, 2015); the greatest variations in full-year seroprevalences were observed among Marine Corps and Navy reservists. As was observed for total civilian applicants, annual seroprevalences among Army active component service members, Navy active component members, Air Force active component members, Navy reservists, and Marine Corps reservists were highest in 2015. Seroprevalences among the Navy Reserve exhibited a pronounced drop after 2015, while full-year seroprevalences among the Army Reserve were relatively stable during the surveillance period. Overall (January 2015–June 2020), across the services, HIV antibody seroprevalences were highest among Army reservists, Army National Guard members, and Navy reservists. Across active and reserve components of all services, seroprevalences continued to be higher among males than females.
There are several limitations that should be considered when interpreting the results of the current analysis. For example, because of the frequency of screening in the military (as an applicant, routinely every 2 years, and before and after overseas deployments), routine screening now detects relatively recently acquired HIV infections (i.e., infections acquired since the most recent negative test of each affected individual). As such, annual HIV-antibody seroprevalences during routine screening of military populations are reflective of, but are not direct unbiased estimates of, incidence rates and trends of acquisitions of HIV infections among military members.
In summary, the U.S. military has conducted comprehensive HIV prevention, education, counseling, and treatment programs for more than 30 years. Since the beginning of these programs, routine screening of all civilian applicants for service and routine periodic testing of all active and reserve component members of the services have been fundamental components of the military’s HIV control and clinical management efforts.9 Summaries of results of screening programs such as those in this report provide insights into the current status and trends of HIV’s impacts in various U.S. military populations.
References
- Centers for Disease Control and Prevention. Kaposi’s sarcoma and Pneumocystis pneumonia among homosexual men—New York City and California. MMWR Morb Mortal Wkly Rep. 1981;30(25):305–308.
- Tramont EC, Burke DS. AIDS/HIV in the U.S. military. Vaccine. 1993;11(5):529–533.
- Brown AE, Brundage JF, Tomlinson JP, Burke DS. The U.S. Army HIV testing program: the first decade. Mil Med. 1996;161(2):117–122.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6130.03, Medical Standards for Appointment, Enlistment, or Induction in the Military Services. 6 May 2018.
- Office of the Assistant Secretary of Defense. Health Affairs Policy Memorandum—Human Immunodeficiency Virus Interval Testing. HA Policy 04-007. 29 March 2004.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense, Instruction 6485.01. Human Immunodeficiency Virus (HIV) in Military Service Members. 7 June 2013.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 1332.45, Retention Determinations for Non-Deployable Service Members. 30 July 2018.
- Army Medical Surveillance Activity. Supplement: HIV-1 in the Army. MSMR. 1995;1(3):12–15.
- Okulicz JF, Beckett CG, Blaylock JM, et al. Review of the U.S. military’s human immunodeficiency virus program: a legacy of progress and a future of promise. MSMR. 2017;24(9):2–7