On an annual basis, approximately 2,500 U.S. Marines and Sailors deploy to Australia on 6-month training rotations. Active duty personnel are generally immunologically naïve to pathogens endemic to tropical Australia, a vulnerability that could significantly impact medical readiness. To estimate risk, we screened 628 post-deployment serum samples by ELISA for serological evidence of infection with Ross River virus, a mosquito-borne alphavirus endemic to tropical Australia. Samples that tested above the negative cutoff value were paired with their pre-deployment samples to identify deployment-related seroconversion. These paired samples were further investigated with a live virus neutralization assay to assess specificity. There was a single RRV seroconversion and 49 false-positive results. In the context of these analyses (i.e., limited sample numbers collected between the months of March and October), we assess the RRV risk to Marine Rotational Force–Darwin as low and encourage strategies such as avoiding and preventing mosquito bites to mitigate the existing risk over widespread vaccination programs, if an FDA-approved vaccine becomes available. The Panbio RRV ELISA lacks the specificity to draw conclusions based on seropositivity from large-scale surveys of U.S. personnel.
What are the new findings?
To our knowledge, this is the first study that examines the rates of seropositivity for Ross River virus in a naïve U.S. Military population prior to an outbreak event. We identified a single seroconversion out of 628 deployers tested.
What is the impact on readiness and force health protection?
Our results, combined with the lack of Ross River virus diagnoses over 11 MRFD rotations, suggest that the current risk to MRFD for Ross River virus infection is low. Strategies such as avoiding and preventing mosquito bites will mitigate the existing risks. These low-cost strategies present a more favorable risk-benefit profile than a widespread vaccination program should an FDA-approved vaccine become available.
Background
Each year, approximately 2,500 U.S. Marines deploy to Australia’s Northern Territory to participate in joint training exercises with the Australian Defence Force, where they will potentially be exposed to a variety of bacterial and viral illnesses not normally encountered by U.S. citizens. Vector-borne illnesses caused by arboviruses such as Ross River virus are common in Australia, including the tropical “Top End.” While not fatal, RRV virus may be characterized by severe symptoms that can last as long as 6 weeks and has the potential to pose a serious threat to force readiness.
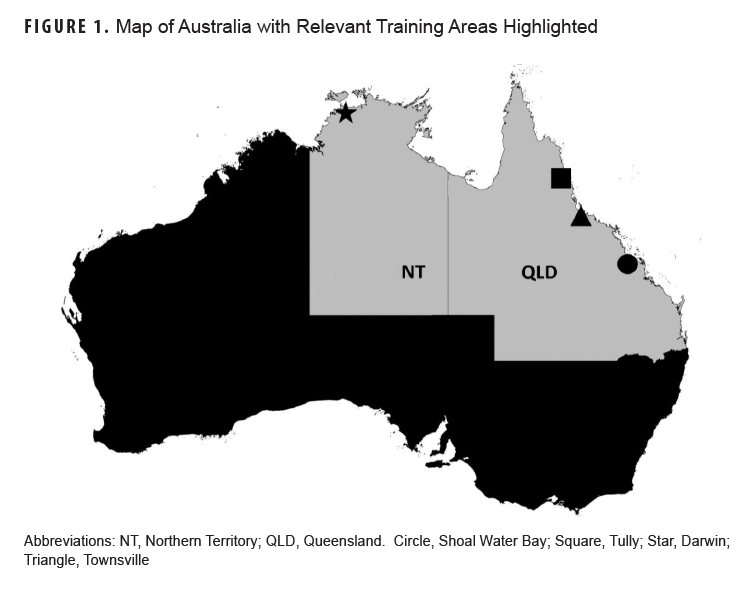
In 2012, U.S. Marines began annual deployments to Darwin, Australia to participate in joint training exercises with the Australian Defence Force and other regional partners.1 While the main body of Marine Rotational Force–Darwin is based in and around Australia’s “Top End” (Figure 1, starred), the east coast of Queensland is also home to an entire company of Marines and numerous training areas (Figure 1, QLD).
While living and training in these areas, U.S. personnel have the potential to encounter a variety of infectious threats not normally encountered by Americans. Burkholderia pseudomallei, for example, is a soil-dwelling bacterial pathogen with a well-documented military relevance.2-8 Vector-borne viruses also have the potential to impact the medical readiness of Marines serving in Australia.
RRV is a mosquito-borne alphavirus unique to Australia and the surrounding islands in the South Pacific and is the most prevalent vector-borne disease in Australia. More similar to Chikungunya virus than Zika, RRV disease is often asymptomatic but is also characterized by fever, malaise, headache, and joint pain. Most individuals recover in a matter of weeks, but pain and temporary disability may last for 3 to 6 months.9-12 While not fatal, RRV disease has the potential to have a significant impact on medical readiness of U.S. personnel in Australia.13,14
Over 20,000 cases of RRV disease were reported in Australia during the 2014-2015 season. This represents an annual rate of 42.4 per 100,000 population, more than double the 5-year mean of 21 per 100,000. The greatest number of cases (6,371) were reported in Queensland, while the Darwin area reported an infection rate of 396 per 100,000.10,15 While the risk of RRV infection in visitors to Australia is generally considered low, the rising incidence of RRV disease within MRFD training areas, combined with immunological naïveté of American personnel, suggests a heightened RRV outbreak potential among U.S. expeditionary forces serving in Australia. In fact, the barracks and training areas along the east coast (Figure 1) have produced RRV outbreaks in Australian Defence Force soldiers and partners.12,14,16 Of note, a joint training exercise in 1997 resulted in at least 8 RRV infections among approximately 9,000 U.S. Marines and Australian Soldiers who had participated in ground exercises in the Shoal Water Bay training area.13,16 The outbreak in 1997 remains the only documented assessment of RRV infection in U.S. expeditionary forces and was generally consistent with the rates of infection for the population of Queensland.12 The purpose of this study was to ascertain the risk of RRV to MRFD and assess the need for rotational pre-exposure prophylaxis to maintain a medically-ready force.
Materials and Methods
Human Specimens
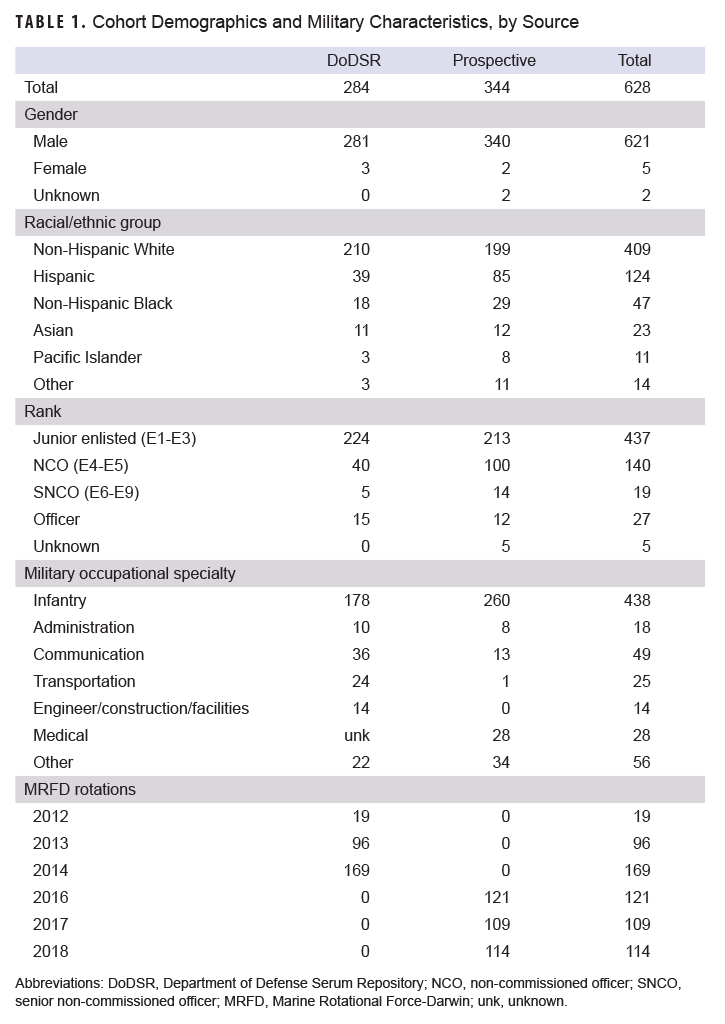
This study was approved by the Naval Medical Research Command Institutional Review Board. As part of a previous study of U.S. Marines deployed to Australia, 1,124 de-identified serum samples were obtained from the Department of Defense Serum Repository, as well as basic demographic data including serum collection dates, sex, military occupational specialty, and deployment history.17,18 For this study, a convenience sample of serum specimens from Marines who deployed to Australia during MRFD rotations between 2012 and 2014 was acquired from 284 individuals with no prior deployment history whatsoever (n=254) or no prior deployments to Australia (n=30). Additional serum samples were collected as part of a prospective observational study of Marines who train in Australia.1 In this study, MRFD deployers participated in pre- and post-deployment activities that included blood sample collection. Additional information including demographics, deployment history, MOS, and training area was self-reported via a study questionnaire. While the previous study was designed to assess the risks of B. pseudomallei to MRFD, all participants selected for this study provided written informed consent for additional testing related to their training in Australia. Serum samples from 344 individuals who participated in MRFD rotations between 2016 and 2018, whose time in Australia included living and/or training in the east coast areas of Australia, were selected for RRV testing. Demographic characteristics of both cohorts are provided in Table 1.
Serology
ELISA
Panbio Ross River Virus IgG ELISA kits (Cat# SD04PE11) were obtained from Alere (QLD 4169, Australia). Post-deployment samples were first screened according to the manufacturer’s instructions. A manufacturer-provided algorithm combines data produced by a series of controls into a lot-specific assay cut-off value that is used to convert specimen absorbance measurements into “Panbio Units.” Measurements below 9 Panbio Units indicate RRV-negative, above 11 indicate RRV-positive, while values between 9 and 11 are equivocal, requiring a retest. Samples producing over 9 Panbio units in the screen were paired with their pre-deployment sera and reassessed further using the same methods.
Micro-Neutralization Assay (MNA)
Serum neutralizing antibodies (Nab) directed against RRV (RRV QML strain, Genbank No. GQ433354), Barmah Forest virus (BH2193, GenBank No. NC_001786), or Chikungunya virus (a CHIKV Reunion strain, GenBank No. DQ443544), were assessed using a micro-neutralization assay, modified according to the methods previously described.19 Anti-BFV, anti-CHIKV, or anti-RRV-specific NAb titers ≥10 were considered positive.
Results
We first sought to identify samples with elevated antibodies to RRV by screening post-deployment sera with the Panbio RRV ELISA kit as described in the Methods. Fifty samples from the screen of 628 post-deployment samples scored above 9 Panbio units, placing them within the equivocal or positive ranges of the assay; 18 of these samples were from the DoDSR cohort (Figure 2a) and 32 samples were from the prospective cohort (Figure 2b).
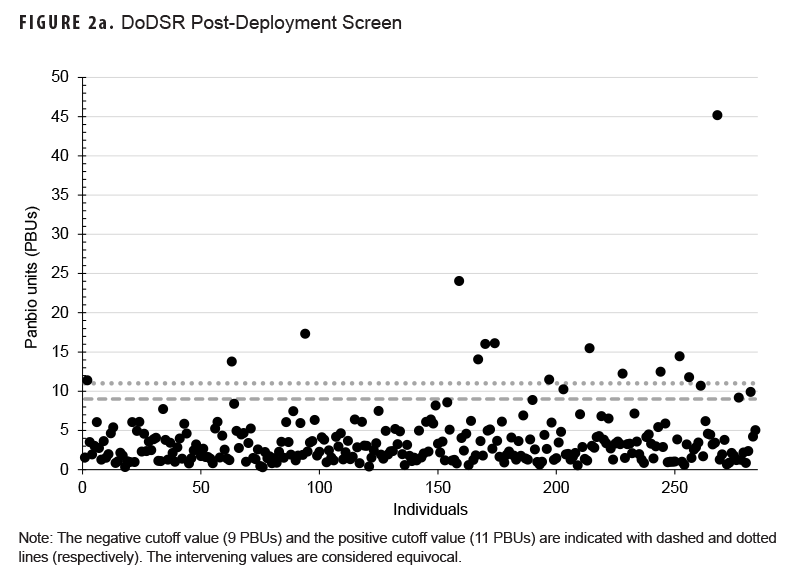
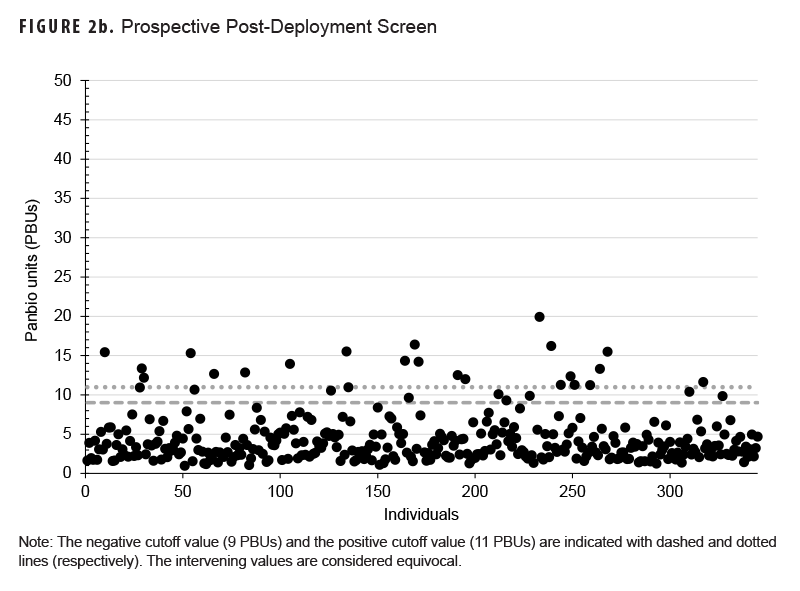
Each of these samples was then paired with its pre-deployment sample, and the assay was repeated to determine if the elevated titers detected in the screen were the result of a deployment-related seroconversion. Samples from the DoDSR cohort of archived specimens yielded a single individual with a potentially significant deployment-related seroconversion (Table 2a), while 2 individuals from the prospectively-collected cohort exhibited potential seroconversion (Table 2b, 59 and 63).
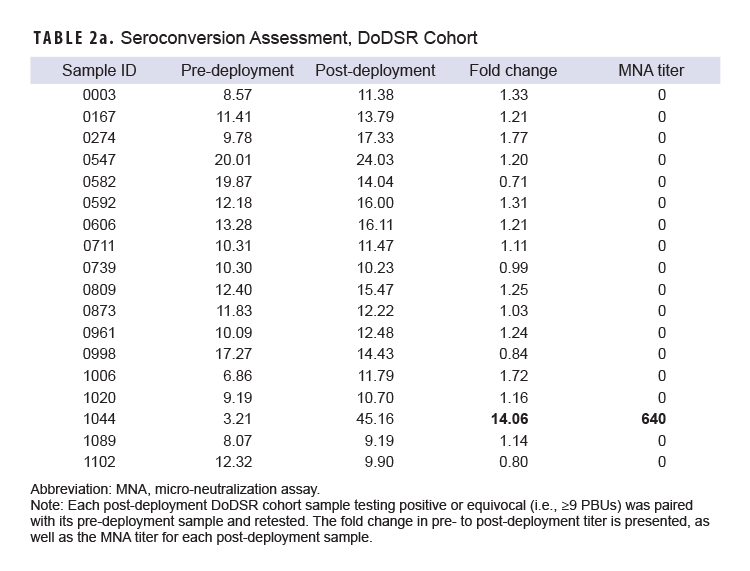
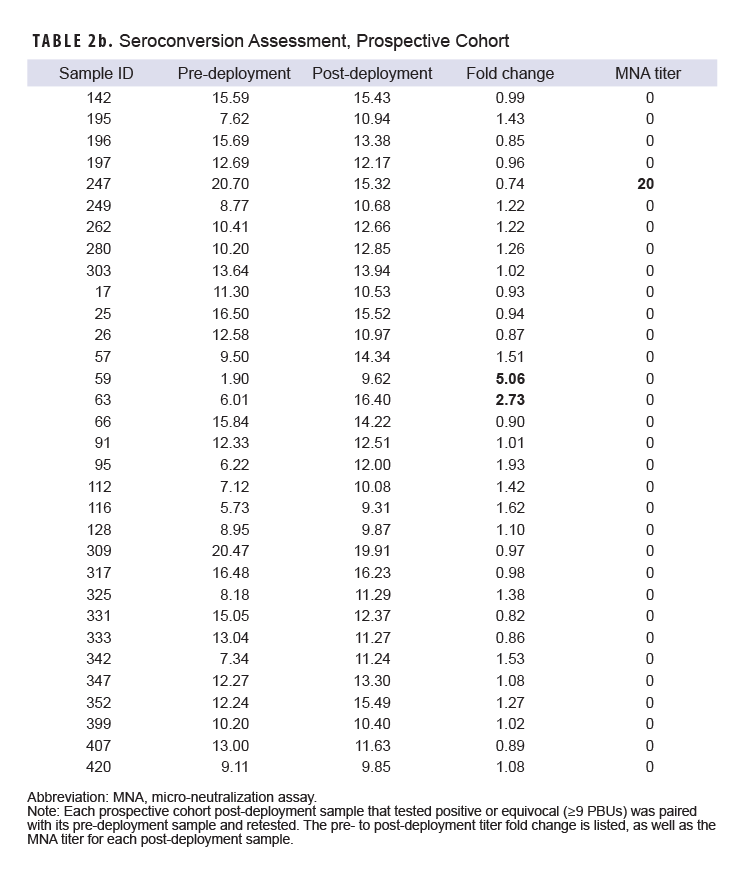
Of the remaining 47 individuals with elevated post-deployment titers, further testing revealed no change from pre-deployment values. Alpha viruses such as RRV, Chikungunya virus, and Barmah Forest virus are known to produce cross-reactive antibodies potentially confounding serological analyses.20 To confirm our results, we assessed the sera’s ability to neutralize RRV in a live virus microneutralization assay (MNA) described in the Methods. The single ELISA-detected seroconversion from our DoDSR cohort was confirmed by MNA to produce an RRV-neutralizing titer (NT) of 640 (Table 2a, subject 1044). Conversely, MNA data did not support either of the 2 potential seroconversions detected by ELISA in the prospective cohort. One individual from the prospective cohort was weakly positive (NT=20) for both the pre- and post-deployment samples in the RRV MNA (Table 2b, subject 247). This individual also produced Chikungunya virus-neutralizing antibodies in both pre- and post-deployment sera (NT=160, each; data not shown). The remaining samples from both cohorts were confirmed negative by RRV MNA. No sample from either cohort neutralized Barmah Forest virus (data not shown).
Discussion
In this study, we combined archived specimens and prospectively collected samples from Marines with the goal of characterizing the risks of RRV infection to American personnel while deployed or training in tropical Australia. While not fatal, RRV poses a vector-borne outbreak threat to U.S. personnel in tropical Australia, with potential impact on MRFD medical readiness.13,14 By combining broad screening of post-deployment samples with targeted assessment of paired, pre- and post-deployment samples, followed by live virus neutralization assays for confirmation, we were able to differentiate between deployment-related seroconversion and false-positive results.
One of the strengths of this study is the sample and demographic collection leveraged from the prospective study of Marines.1 Study questionnaires allowed for the identification of specific training areas (Figure 1), as opposed to the country-level deployment histories provided with the DoDSR specimens. The most notable limitation of this work was sample size. Each year approximately 2,500 expeditionary forces deploy to Australia, making this sample set small in comparison to the number of Marines deployed to Darwin over the years.
An important finding in this study is the apparent lack of specificity in the Panbio RRV ELISA kits. Results from approximately 8% (50/628) of post-deployment samples were either positive (n=36) or equivocal (n=14). Further examination revealed that pre-deployment sera from 36 of these individuals also tested above the assay’s negative threshold. This was particularly interesting, considering that only 1 of those individuals had a travel history outside the continental U.S. When these samples were investigated with a more specific live virus neutralization assay, only 1 individual tested weakly positive (NT=20) in both pre- and post-deployment samples (Table 2b, subject 247). Further investigation of these samples, however, revealed prior Chikungunya virus infection, which was previously demonstrated to elicit antibody responses that cross-react with RRV, further questioning the utility of this low-specificity ELISA assay.20 The 14-fold increase in RRV titer observed in subject 1044 (Table 2a), however, was confirmed by RRV MNA, indicating a single deployment-related seroconversion. The remaining 48 non-negative samples represent, at a minimum, 34 false-positive results (6% false-positive rate) and 14 equivocal results (rate of 2.4%). These data should urge caution when attempting to draw conclusions based on seropositivity from large-scale surveys of U.S. personnel with unproven assays and underscore the need for specific confirmatory testing of potentially positive results.
To our knowledge, this is the first study to proactively examine the rates of seropositivity for RRV in a naïve U.S. military population, and the second study of RRV in expeditionary forces overall.13 The previous study detailed an outbreak that occurred during a joint training exercise in 1997. A combination of acute manifestation and post-exercise surveillance identified at least 8 RRV infections among the approximately 9,000 U.S. and Australian service members who participated in ground exercises around the Shoal Water Bay training area (Figure 1). While this event highlights the potential impact of RRV on expeditionary forces, the exercise occurred during the rainy season and peak vector activity. Furthermore, none of the infected individuals complied with recommended personal mitigation strategies, i.e., permethrin-treated uniforms, DEET repellent, bed netting, etc. While MRFD is housed and trained in areas known to experience outbreaks, MRFD arrives in Australia in the late-March or April timeframe, and training operations occur almost exclusively during the dry season.10 To highlight the importance of seasonality, the past 11 MRFD rotations combined vastly exceed 9,000 participants yet produced 0 RRV diagnoses, and this study identified only 1 seroconversion. These facts combine to suggest that the current risk to MRFD for large-scale RRV infection is quite low. Strategies for avoiding and preventing mosquito bites such as permethrin-treated uniforms, insect repellent, and command emphasis on their proper use should mitigate existing risks.21,22 Meanwhile, MRFD is scheduled to return to Australia for decades to come and may include a year-round presence. The MRFD force health protection posture will likely change during that time. Medical leadership should continue to monitor MRFD personnel for infectious agents uniquely endemic to Australia and keep these infections in mind when clinical presentations warrant.
Acknowledgements
We thank Mark Mayo for invaluable logistical support.
Author Affiliations
The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc.: Mr. Bell and Mr. Hulsey; Australian Defence Force Malaria and Infectious Disease Institute, Enoggera, Queensland, Australia: Dr. Liu; Austere Environments Consortium for Enhanced Sepsis Outcomes, Biological Defense Research Directorate, Naval Medical Research Command-Frederick, Ft. Detrick, Maryland: Dr. Schully.
Funding
This study was funded by the Armed Forces Health Surveillance Division Global Emerging Infections Surveillance Branch, ProMIS ID P0135_18_NM and 20160500210.
Disclaimers
The study protocols were approved by the Institutional Review Boards of the Naval Medical Research Command in compliance with all applicable U.S. Federal regulations governing the protection of human subjects.
The views expressed in this article reflect the results of research conducted by the authors and do not necessarily reflect the official policy nor position of the Department of the Navy, Department of Defense, or the United States or Australian governments.
Kevin L. Schully is a federal employee of the U.S. Government. This work was prepared as part of official duties. Title 17 U.S.C. 105 provides that “copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
References
- Chan-Cuzydlo A, Harrison DJ, Pike BL, et al. Cohort profile: a migratory cohort study of US Marines who train in Australia. BMJ Open. 2021;11(9):e050330. doi:10.1136/bmjopen-2021-050330
- Spotnitz M. Disease may be Vietnamese time bomb. Medical World News. 1966;7:55.
- Sanford JP, Moore WL, Jr. Recrudescent melioidosis: a Southeast Asian legacy. Am Rev Respir Dis. 1971;104(3):452-453. doi:10.1164/arrd.1971.104.3.452
- Mackowiak PA, Smith JW. Septicemic melioidosis: occurrence following acute influenza A six years after exposure in Vietnam. Case reports. JAMA. 1978;240(8):764-766.
- Mays EE, Ricketts EA. Melioidosis: recrudescence associated with bronchogenic carcinoma twenty-six years following initial geographic exposure. Chest. 1975;68(2):261-263.
- Johnson AB, Ali N. Reactivation of latent melioidosis. Case reports. Postgrad Med J. 1990;66(779):732-733.
- Koponen MA, Zlock D, Palmer DL, Merlin TL. Melioidosis: forgotten, but not gone! Case reports. Arch Intern Med. 1991;151(3):605-608.
- Larson DT, Schully KL, Spall A, Lawler JV, Maves RC. Indirect detection of Burkholderia pseudomallei infection in a US marine after training in Australia. Open Forum Infect Dis. 2020;7(5):ofaa103. doi:10.1093/ofid/ofaa103
- Harley D, Sleigh A, Ritchie S. Ross River virus transmission, infection, and disease: a cross-disciplinary review. Clin Microbiol Rev. 2001;14(4):909-932. doi:10.1128/CMR.14.4.909-932.2001
- Knope K, Doggett SL, Jansen CC, et al. Arboviral diseases and malaria in Australia, 2014-15: annual report of the National Arbovirus and Malaria Advisory Committee. Commun Dis Intell (2018). 2019;43. doi:10.33321/cdi.2019.43.14
- Fraser JR. Epidemic polyarthritis and Ross River virus disease. Clin Rheum Dis. 1986;12(2):369-388.
- Shanks GD. Could Ross River virus be the next zika? J Travel Med. 2019;26(5). doi:10.1093/jtm/taz003
- Yund J, Montville MR, Cope SE, Hueston L, Russell RC, Parker GS. Ross River virus disease (“epidemic polyarthritis”), Exercise Tandem Thrust 97, Queensland, Australia, March 1997. MSMR. 1997;3(7):13-15.
- Liu W, Kizu JR, Le Grand LR, et al. Localized outbreaks of epidemic polyarthritis among military personnel caused by different sublineages of Ross River virus, northeastern Australia, 2016-2017. Emerg Infect Dis. 2019;25(10):1793-1801. doi:10.3201/eid2510.181610
- Qian W, Hurst C, Glass K, Harley D, Viennet E. Spatial and temporal patterns of Ross River virus in Queensland, 2001-2020. Trop Med Infect Dis. 2021;6(3). doi:10.3390/tropicalmed6030145
- Hueston L, Yund A, Cope S, et al. Ross River virus in a joint military exercise. Commun Dis Intell. 1997;21:193.
- Rubertone MV, Brundage JF. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002;92(12):1900-1904.
- Schully KL, Burtnick MN, Bell MG, et al. Serological evidence of Burkholderia pseudomallei infection in U.S. Marines who trained in Australia from 2012-2014: a retrospective analysis of archived samples. MSMR. 2019;26(7):8-17.
- Raharjo E, Tadano M, Okamoto Y, Okuno Y. Development of a micro-neutralization test for chikungunya virus. Biken J. 1986;29(1):27-30.
- Kam YW, Pok KY, Eng KE, et al. Sero-prevalence and cross-reactivity of chikungunya virus specific anti-E2EP3 antibodies in arbovirus-infected patients. PLoS Negl Trop Dis. 2015;9(1):e3445. doi:10.1371/journal.pntd.0003445
- Harley D, Ritchie S, Bain C, Sleigh AC. Risks for Ross River virus disease in tropical Australia. Int J Epidemiol. 2005;34(3):548-555. doi:10.1093/ije/dyh411
- Armed Forces Pest Management Board. 36 Personal Protective Measures Against Insects and Other Arthropods of Military Significance. 2015.