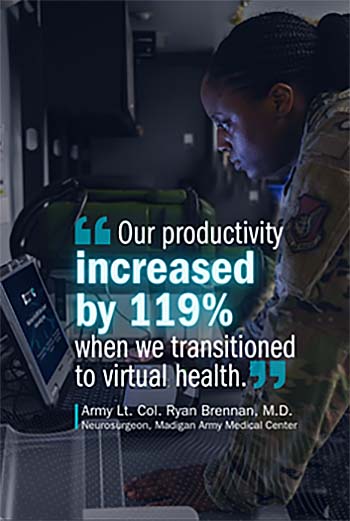
 "Our productivity increased by 119% when we transitioned to virtual health." (Photo by Connected Health)
"Our productivity increased by 119% when we transitioned to virtual health." (Photo by Connected Health)
Secure and Convenient
So – why the move to MHS Video Connect?
Early in the pandemic, health care systems across the world struggled to balance providing care with having face-to-face patient engagements.
Within the MHS, virtual health options authorized and employed early in the pandemic had technical limitations, including unnecessary security risks, and incompatible with patients' web browsers or devices.
MHS Video Connect eliminates these issues, and facilitates a much more streamlined process.
Through a few simple clicks, the provider and patient 'enter' their own secure, private virtual treatment room. MHS Video Connect provides real-time access to care, from almost anywhere with internet access, and it works with existing MHS medical processes and electronic health records.
Virtual health also offers providers more control in their day-to-day lives — and that is always something we like. As a provider, I can now determine when I want to see someone virtually. For example, I can see patients without the challenges of clinic delays due to traffic or limitations in our physical space. It has also offered me the opportunity to see, and treat patients on a schedule that is convenient for me.
One of the biggest advantages to providers is that virtual health remains a moldable medium. It can be adapted to fit your practice and convenience needs in nearly endless ways.
Patients have shared with me that they love the simple and easy access to their doctors without the potential hassle of taking time off work, scheduling child care, traveling to the clinic and then sitting in waiting rooms.
MHS Video Connect is easy, intuitive, and does not take much to learn. Once you are on it, you may find that it is something you enjoy doing.
Saving Money, Resources, and Lives
MHS Video Connect's advantages extend beyond improved readiness, access, and convenience. Using the system also yields huge cost savings and increased efficiency in the use and expenditure of finite resources.
For our patients in Alaska, the cost of temporary duty travel to our medical center can be costly and often runs between $25,000 and $50,000. Every virtual visit that determines that a patient does not need to travel may save up to $1,500 a day, per visit.
Virtual health may also have significant, but less easily quantified, value through a reduction in productivity loss, reduced number of duty days lost to travel to appointments, and provides an overall improvement in mission readiness. Taken together, these factors directly serve the MHS mission of creating a medically ready force.
Using MHS Video Connect may also alleviate some of the resource constraints that we have in clinic. When we are limited in both physical space and personal protective equipment, the platform allows us to facilitate greater numbers of patient visits in a single day. While I am doing a virtual visit, my colleagues can see patients physically in clinic, which can immediately double the number of patients our clinic can treat in a day.
By increasing the number of visits available in a day, we are also able to radically reduce the overall time it takes patients to access care. This increase in access is critically important during these challenging times.
Additionally, managing the number of beneficiaries physically entering the clinic is essential to keeping providers, care teams, and patients safe. Increasing virtual appointments helps to reduce foot traffic and reduces unnecessary exposure to COVID-19 and other pathogens.
Investment in the Future
One of the things that became clear from the start of the COVID-19 pandemic was that virtual health is rapidly becoming an integral part of maintaining a functioning medical service. Given its popularity with providers and patients alike, virtual health is something that is here to stay.
Providers should be open-minded and embrace virtual health — and MHS Video Connect in particular — because it is such a great avenue for facilitating patient care. With anything new, of course, there may be growing pains and a learning process. But my experience with virtual health and MHS Video Connect is that they have made things easier for me and my staff. I think most providers will find that once they begin the process of using virtual health, both they and their patients will appreciate the investment going forward.